











 Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.
Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.

Background: Herlyn-Werner-Wunderlich Syndrome or OHVIRA syndrome is uterine didelphys with obstructed hemi-vagina and ipsilateral renal agenesis syndrome is a very rare congenital urogenital anomaly.
Case: A 21-year-old female presented with acute abdomen and severe dysmenorrhea. Ultrasonography performed in obstetric emergency room showed a cystic lesion in right pelvic area, free fluid in Douglas’s pouch and right renal agenesis. Diagnostic laparoscopy revealed uterine didelphys with right ovarian hemi-torsion. A unilateral hysterectomy was conducted.
Conclusion: HWW syndrome could manifest as acute abdominal symptoms and typically requires treatment involving resection of the vaginal septum and drainage of hematometrocolpos.
Herlyn-Werner Wunderlich (HWW) syndrome is a rare congenital Mullerian duct anomaly of the female urogenital tract characterized by uterus didelphys and obstructed hemi-vagina and ipsilateral renal agenesis (OHVIRA) syndrome (1). It usually occurs at puberty and presents after menarche with vague symptoms such as recurrent pelvic pain or dysmenorrhea during menses secondary to haematocolpos and rarely urinary incontinence or urine retention may accompany (1). During examination, a visible bulge on the vaginal sidewall may be observed, leading to a diagnosis of obstructed hemivagina and the presence of a second cervix. This condition often coincides with a uterine anomaly, which has been categorized in various studies as uterus didelphys or duplicated uterus. Although the classic presentation includes ipsilateral renal agenesis, recent series have reported rare instances of patients having two kidneys, and a study from Finland identified cases with a rectovesical band (2).
The incidence of OHVIRA is reported to be approximately 1 in 20,000 cases (3). Because it’s so rare, diagnosis is tough to make without the help of imaging techniques. That’s why the physician must suspect a uterine anomaly if the patient presents with progressive pelvic pain during menses and is accompanied by renal agenesis (4). Accurate diagnosis of Müllerian duct anomalies is crucial because of the higher incidence of associated conditions like endometriosis, menstrual irregularities, infertility, and obstetric complications (5). It is important to not overlook the management of patients before puberty due to various potential issues. Herein, we describe the case of a 21-year-old female with OHVIRA syndrome who presented to the emergency room with an acute abdomen.
A 21-year-old female with severe pelvic pain, accompanied by nausea and vomiting presented to the emergency room. The patient reported having irregular menses with dysmenorrhea since her menarche at 14 years old and this being the worst of all. She stated that she has been married for 2 years and has dyspareunia. She complained of missing her period in her recent menstrual cycle and having progressive pelvic pain that was nonresponsive to several nonsteroidal painkillers for three days.
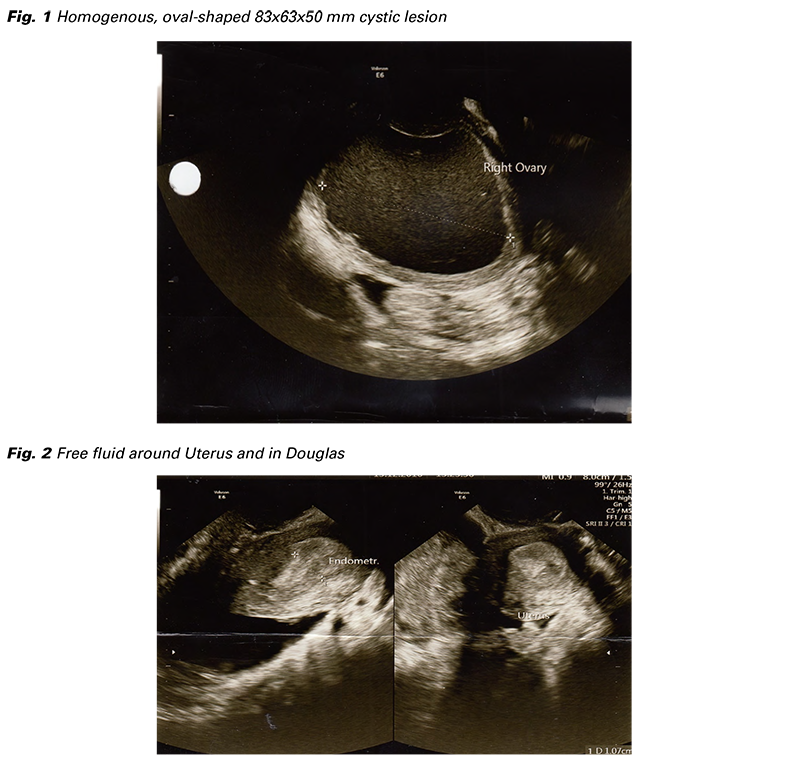
Physical examination revealed tenderness, defense, and palpable pelvic mass in the right lower quadrant. A speculum examination demonstrated a nulliparous single cervix with one vagina. All the laboratory testing was normal except for WBC: 18.000, CRP 49, and Ca-125: 65. Other tumor markers and beta-hCG were negative. Ultrasound revealed a homogenous, oval-shaped 83x63x50 mm cystic lesion in the right intra-abdominal region lacking vascularity (Fig. 1). The left ovary was normal and 45 mm of fluid in the pouch of Douglas (Fig. 2). The right kidney was not visualised by abdominal ultrasound. Our clinic lacked further imaging options and acute abdomen could not be ruled out, so, a diagnostic laparoscopy was planned to rule out ruptured endometrioma or ovarian torsion.
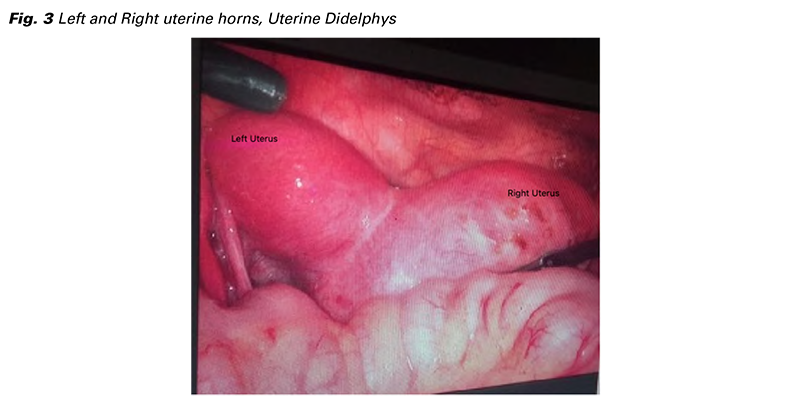
In laparoscopy, two uterine horns were separate and compatible with uterine didelphys (Fig. 3). The left uterus, the left ovary, cervix, and vagina were normal. The right one is almost double in size and filled with blood consistent with hematocolpos. The right ovary was hemi-torsioned accompanied with endometriotic focii in the right adnexa. There was about 50 cc of serohemorrhagic fluid in Douglas’s pouch. Laparoscopic detorsion was performed and then the surgery was converted to laparotomy. The right-side uterus was opened, and the hematometra was drained with suction. A ring forceps was tried to place through the uterine cavity down to the cervix, but the endocervical canal was non-communicating with the right-side uterine cavity. Hysteroscopy was performed to check the cervix and vagina. The obstructed hemi-vagina on the right side was visualized. A unilateral right hysterectomy was performed.
No complications were observed. She was discharged on the postoperative 2nd day. At the fourth month’s follow-up visit, she had no complaints of severe dysmenorrhea and had regular menses every month. Her complaint of dysparonia was decreased but not totally disappeared. This can be related to endometriosis.
Informed consent was obtained from the patient to publish the case report.
The female reproductive system originates from the Müllerian ducts during embryogenesis, which will form the uterine tubes, uterus, and the upper two-thirds of the vagina. If one of the ducts fails to develop, only one Müllerian duct contributes to the development of the uterus. This developmental anomaly is classified based on its relationship with the uterine cavity and divided into four groups by the American Society for Reproductive Medicine (ASRM): unicornuate uterus with a communicating rudimentary horn, unicornuate uterus with a noncommunicating rudimentary horn, isolated unicornuate uterus, and unicornuate uterus with a noncommunicating, cavitary rudimentary horn (6). Unicornuate uterus with a rudimentary horn is a rare form of Müllerian duct anomaly. Its incidence is 0.06% (7). In 83% of cases, the rudimentary horn is noncommunicating (8). This pathology can be diagnosed incidentally during a gynecological examination or as seen in our case, during surgical intervention for acute abdomen. These patients‘ possible causes of abdominal pain include hematometra, pyometra, and torsion (9). Another cause of abdominal pain is endometriosis (10). In these cases, retrograde menstruation develops from the ipsilateral tube, supporting the theory of retrograde menstruation in endometriosis. As seen in our case, concomitant endometriosis can lead to severe dysmenorrhea, chronic pelvic pain, and dyspareunia (10). Müllerian anomalies are often associated with the absence or gross malformation of the renal tract. Renal agenesis on the same side is seen in 40% of patients with a unicornuate uterus (11). A uterine or Müllerian anomaly should raise suspicion for cloacal, spinal, and renal anomalies (12). Meticulous examination and imaging play a significant role in detecting and classifying Müllerian anomalies, ensuring appropriate management. Although many of these abnormalities can be diagnosed with hysterosalpingography or sonography, MRI is close to 100% accurate in detecting Müllerian anomalies (13). Therefore, MRI is considered the preferred diagnostic method due to its superior sensitivity in detecting uterine morphology and vaginal continuity compared to ultrasonography. Complex and renal anomalies, along with secondary findings of endometriosis, are best detected noninvasively. Our clinic lacks MRI technique that led us to perform the surgery unprepared and without knowing patient’s anomaly thoroughly. Treatment typically involves resecting the vaginal septum and draining the hematometrocolpos. If septum resection is not feasible or recurrent stenosis occurs, unilateral hysterectomy is preferred (14). Due to the risk of ascending infection, it is not recommended to perform a simple incision and drainage of the obstructed hemivagina. In an article which was published in Fertil Steril in 2007, management of twenty-seven of OHVIRA case series were retrospectively investigated and concluded that the majority of cases of OHVIRA syndrome can be effectively managed with a single stage vaginoplasty (15). Routine laparoscopy is typically unnecessary for treatment if the diagnosis is known beforehand and the patient is not presented with acute abdomen.
There are very few case reports of HHW presented with acute abdomen as in our case.
The existing data is in the form of case reports and generally presents as surgical emergencies. In the clinic, many cases receive a diagnosis of early menarche. However, as in our case, some cases can also receive a diagnosis of acute abdomen upon presenting to the emergency room at older ages. We wanted to emphasize the importance of MRI to establish an early diagnosis of the HWW to avoid serious complications and prevent an emergency surgery. Also, it is crucial to suspect of HWW in such cases to manage a proper follow up and right surgical intervention to ensure fertility.