











 Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.
Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.

Dysmenorrhea, derived from Greek, which translates to “painful monthly bleeding” refers to pain experienced during the menstrual cycle (1). Dysmenorrhea is the prevalent issue affecting female individuals of reproductive age often leading to substantial emotional, psychological, and functional health challenges. It is a widespread gynaecological issue that can significantly affect a patient’s quality of life (1).
Dysmenorrhea is categorised into two types: primary and secondary. Primary dysmenorrhea is characterised by recurring lower abdominal pain during menstruation due to uterine contraction that is not associated with any other medical conditions and typically begins within a year of menarche such as painful menstrual crumps in teenagers. On the other hand, secondary dysmenorrhea is associated with identifiable underlying conditions, such as pelvic diseases, and typically arises more than two years after menarche such as painful periods due to endometriosis where endometrial tissue grows outside the uterus leading to chronic pelvic pain (2). Dysmenorrhea, characterised by sharp, spasmodic, and intermittent pain, is a common issue that affects women globally. It is classified based on its impact on daily activities: mild if it does not hinder them, moderate, and severe if it prevents them entirely. The physical symptoms include headaches, fatigue, sleep disturbances, breast tenderness, various body aches, appetite changes, nausea, vomiting, constipation or diarrhea, and increased urination. Additionally, dysmenorrhea can also cause psychological symptoms such as anxiety, depression, and irritability (3).
In Malaysia, primary dysmenorrhea prevalence reached a significant rate of 62.3% (4). This condition is a major source of gynaecological morbidity, impacting women’s ability to concentrate and perform daily activities. In severe cases, it can lead to psychological problems such as depression and reduced social interaction (5). In Malaysia, dysmenorrhea plays a role in reducing concentration and increasing absenteeism from school or work (4). It was more common in younger individual aged 18-24 years in Malaysia and the prevalence varied among ethnic groups, with the studies indicated that higher rates in Malay compared to Chinese and Indian population (6,7). Based on the findings, underweight and obese individuals were more likely to experience dysmenorrhea compared to those with a normal BMI (7). It has a negative impact on women’s activities and reproductivity. According to previous studies, there was the moderate negative correlation between physical activity and severity of dysmenorrhea (r = -0.48, p < 0.035) indicated that individuals met with WHO physical activity guidelines, reported lower pain severity (6). The problem was further exacerbated by a widespread lack of knowledge about dysmenorrhea among women. Many are unaware of effective management strategies and proper menstrual hygiene practices, leading to inadequate care and exacerbating their condition. This lack of understanding can significantly affect their quality of life, influencing both academic achievements and workplace performance. Moreover, studies indicated that cultural stigmas surrounding menstruation may affect management and understanding dysmenorrhea since knowledge about menstruation usually transmitted through mothers or school system rather than fathers or internet sources (8). To address these issues, it is crucial to improve education and awareness about dysmenorrhea, enabling better management and reducing its overall impact (4).
Apart from this inefficient and poor management of dysmenorrhea often involves improper use of medication, which can lead to serious comorbidities. For instance, excessive use of painkillers to alleviate abdominal cramps and pain may increase the risk of renal impairments or gastrointestinal bleeding (4). In severe cases, these complications can be potentially life-threatening.
Understanding the prevalence and impact of dysmenorrhea is crucial, as it highlights the need for effective management strategies and greater awareness. Despite its high prevalence and its significant effect on quality of life, dysmenorrhea remains under-recognized and often inadequately addressed in healthcare settings. Therefore, the aim of our study was to identify the prevalence of dysmenorrhea among 18- to 50-year-old adult females in Malaysia and its impact on the quality of life and their daily functioning to learn about coping strategies according to severity of dysmenorrhea.
Study design, setting and study population
The study design was an analytical cross-sectional study which was conducted during 2024. Study focuses on Malaysian adult females aged 18 to 50 years old who are accessible to WhatsApp, Telegram, Instagram, email and who can comprehend English and/or Bahasa Melayu. According to previous literature, the study population was adult females aged 18 to 50 years old who reside in Malaysia, regardless of their socio demographic background.
Data collection and Sample size determination
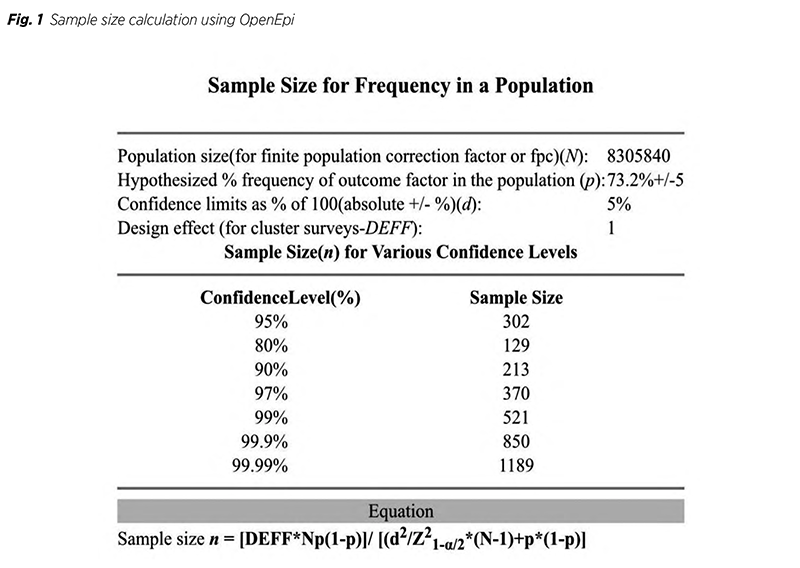
The sample size for this study was calculated using OpenEpi (Version 3.01). The estimated prevalence of dysmenorrhea among females aged 18 to 50 years old in Malaysia was 73.2% (9). The confidence limit was set to +/- 5 and based on that with the 95% of confidence level, and 5% precision, the estimated sample size calculated was 302 as shown in Figure 1. By considering a non-response rate of 20%, the final required sample size was approximately 378.
This study used non-probability convenience sampling to recruit participants. This approach ensured practicality by selecting medical students who are readily accessible or willing to participate. Data collection was conducted through an online questionnaire adapted from pre-existing, validated sources, and it was available in both English and Bahasa Malaysia. The questionnaires consisted of eight sections with 54 questions which were adapted mainly from the published articles done by Mizuta R et al. (2023) and Abreu-Sánchez A. et al. (2020), cited from credible sources to support the findings and both articles presented with balanced information instead being overly biased or onesided (10, 11). In this study, we conducted content validation and calculated the Content Validity Index (CVI) for the questionnaire to strengthen the face and content validity of the questionnaire for meaningful and understandable to the targeted population since this process included expert evaluation and CVI score was 0.95 indicated the evidence of good content validity of the research questionnaire.
Section 1 provided an information sheet and informed consent, informing participants about the study, its voluntary nature, and potential risks. Section 2 gathered sociodemographic information, including age, weight, height, nationality, ethnicity, education level, occupation, economic status, and living environment. Section 3 consisted of questions about severity of dysmenorrhea which was characterized into four categories such as no dysmenorrhea, mild, moderate and severe dysmenorrhea, using a visual analogue scale from 1-10 for pain intensity. Section 4 examined triggers or situations that intensified menstrual pain, such as pain with a full bladder or bowel movements, where participants rated the pain from 1-10 or selected “none” if not experienced.
Section 5 addressed how dysmenorrhea interfered with their daily life, education, and social activities, with “Yes,” “No,” or “Not applicable” responses. Section 6 explored menstrual symptoms (e.g., nausea, vomiting, fatigue) and whether they led to absenteeism. Section 7 covered lifestyle habits such as smoking, sleep duration, breakfast consumption, snacking habits, and weekly exercise. Lastly, Section 8 focused on coping strategies for dysmenorrhea, including the use of analgesics, oral contraceptives, or seeking medical consultation, with “Yes” or “No” options provided for each strategy.
Sampling Method
In this study, non-probability convenience sampling method was used to recruit the participants. In order to collect responses, we shared a survey link to family, friends, neighbours, public adult audience and associates on various social media platforms, including WhatsApp, Instagram, Facebook, Telegram, and through email. The study includes Malaysian female participants who are 18 to 50 years old, of any ethnicity, and willing to take part. The females who have reached menopause, aged less than 18 yrs and above 50 and those who did not provide informed consent were excluded from the study.
Data Processing and Data Analysis
The data were processed and analysed using the SPSS (Version 29) software and the results were presented through frequency counts and other descriptive statistics. Under the inferential statistics, chi-square test for analysis was selected to measure the association between independent and dependent categorical variables. The significant level (p-value) was set up at 0.05 with 95% confidence interval.
Ethical Consideration
An information document outlined the goal of the study, its voluntary nature, and the lack of reward is given to participants. In order to ensure understanding and the freedom to withdraw at any moment, written informed permission was provided prior to enrolment of the study. Anonymized data were safely preserved, with only the research team having access to the data. The ethical approval was obtained from research management Research Ethics Committee, Manipal University College Malaysia (MUCM). (Ref: MUCM/ Research Ethics Committee – 001B/08/2024)
Descriptive data of questionnaire
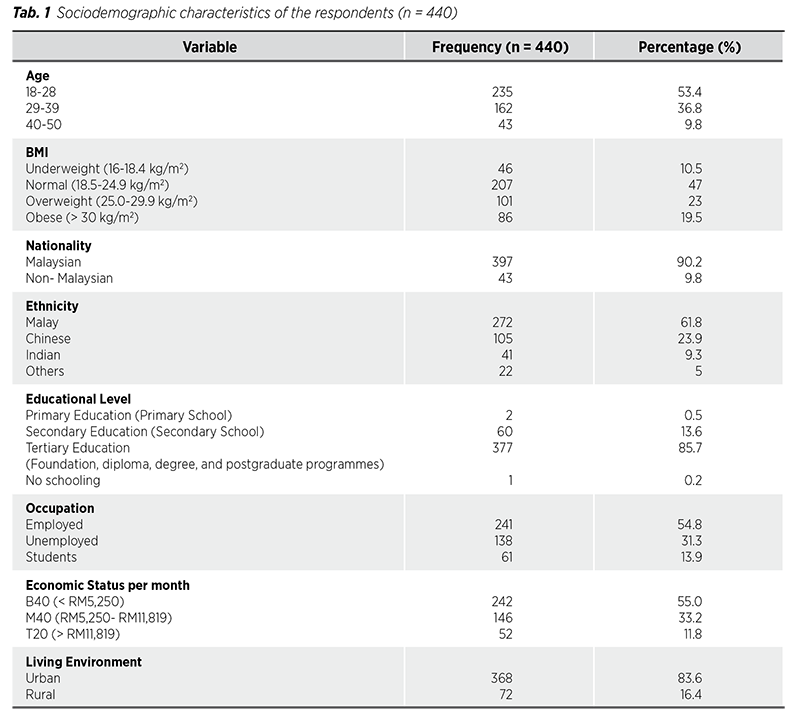
The age distribution showed that 53.4% were aged 18-28, 36.8% were 29-39, and 9.8% were 40-50. The BMI categories indicated that 10.5% were underweight, 47% were normal, 23% were overweight, and 19.5% were obese. Nationality data showed that 90.2% were Malaysian, while 9.8% were non-Malaysian. Ethnicity groups showed that the majority were 61.8% Malay, followed by 23.9% Chinese, 9.3% Indian, and 5% were from other ethnicities. Educational levels showed that 85.7% had tertiary education, 13.6% had secondary education, and only 0.5% had primary education. Employment status revealed that 54.8% were employed, 31.3% were unemployed, and 13.9% were students. Economic status categorized participants as B40 (55%), M40 (33.2%), and T20 (11.8%). Living environment showed a predominance of urban residents at 83.6%, compared to 16.4% in rural areas.
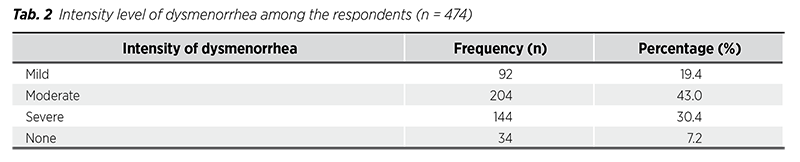
Table 2 presented that 92.8% of the participants suffered dysmenorrhea among 474 respondents, which was the initial total number of respondents. The majority of participants (43%) reported experiencing moderate dysmenorrhea, followed by 30.4% who experienced severe dysmenorrhea. A smaller proportion, 19.4%, had mild dysmenorrhea, while 7.2% of the respondents reported no symptoms of dysmenorrhea at all. This data showed a significant variation in the level of severity due to dysmenorrhea among females aged 18 to 50 years old in Malaysia. This finding rejected the null hypothesis which stated that there was no significant variation in the level of severity among respondents. It was important to note that we cleared the “none” responses, which left us with a final total sample of 440.
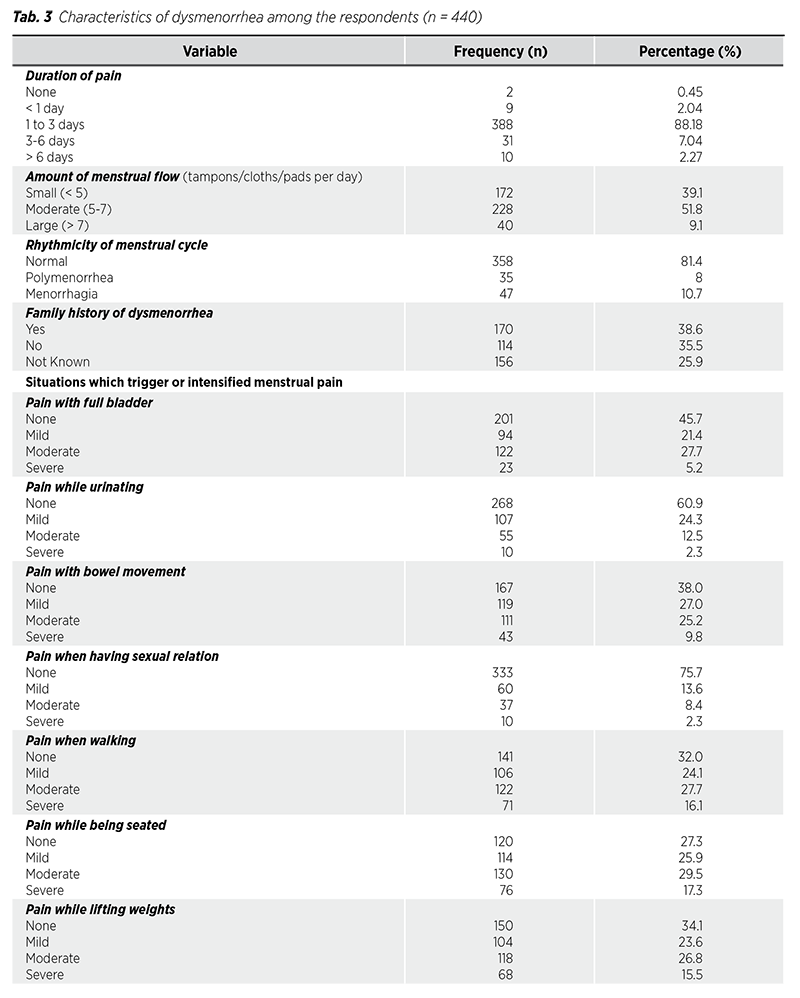
According to Table 3, the duration of menstrual pain was predominantly experienced by individuals for 1 to 3 days, with 388 individuals reporting this timeframe; only a small number experienced pain that lasted longer, and very few reported pains extending beyond 6 days or none at all. Regarding menstrual flow, most individuals experienced a moderate amount (51.8%), while fewer reported either small or large volumes. In terms of cycle rhythmicity, the majority had a normal menstrual cycle (81.4%), with a smaller percentage experiencing menorrhagia or polymenorrhea. Additionally, a notable proportion of individuals (38.6%) had a family history of dysmenorrhea, although there was also a significant number whose family history remained unknown (25.9%).
Most individuals reported experiencing no pain (45.7%) or only mild discomfort when their bladder was full, although a significant number also experienced moderate pain (27.7%), with severe pain being relatively uncommon. During urination, the majority (60.9%) did not experience pain, with only a small fraction reporting moderate to severe discomfort. In terms of bowel movements, while many did not experience significant pain (38%), mild pain (27%) was the most common, followed closely by moderate pain (25.2%), with severe pain occurring less frequently. When it came to sexual relations, a large majority (75.5%) reported no pain, making severe discomfort rare. Pain while walking ranged from mild (24.1%) to moderate (27.7%), with a noteworthy portion experiencing severe pain. For those seated, moderate pain was most reported (29.5%), though mild and severe pain were also observed. Finally, when lifting weights, moderate pain (26.8%) was frequently reported, while severe pain occurred less often.
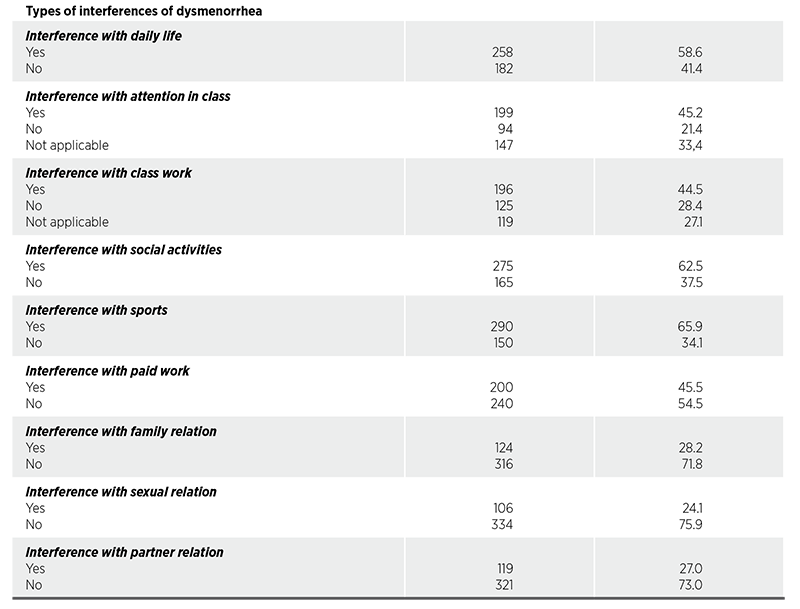
The study also highlighted several ways dysmenorrhea interfered with different aspects of life. A majority of respondents (58.6%) reported that their daily life was disrupted, while 41.4% experienced no such issues. Regarding attention in class, 45.2% had difficulty focusing, 21.4% did not, and 33.4% indicated the question didn‘t apply to them, likely because they weren’t students. Similarly, 44.5% experienced interference with classwork, 28.4% did not, and 27.1% found the question irrelevant. Social activities were impacted for 62.5% of respondents, while 37.5% reported no issues. Sports participation was affected for 65.9%, with 34.1% unaffected. When it came to paid work, 45.5% faced interference, while 54.5% did not. Family relations were affected for 28.2%, but the majority (71.8%) reported no disruptions. Sexual relations were impacted for 24.1%, with 75.9% experiencing no interference, and partner relations were affected for 27% of respondents, while 73% did not face any issues in this area. This showed that dysmenorrhea had a significant impact on daily activities among respondents, which rejected the null hypothesis that stated dysmenorrhea does not have a significant impact on daily activities among females aged 18 to 50 years old in Malaysia.
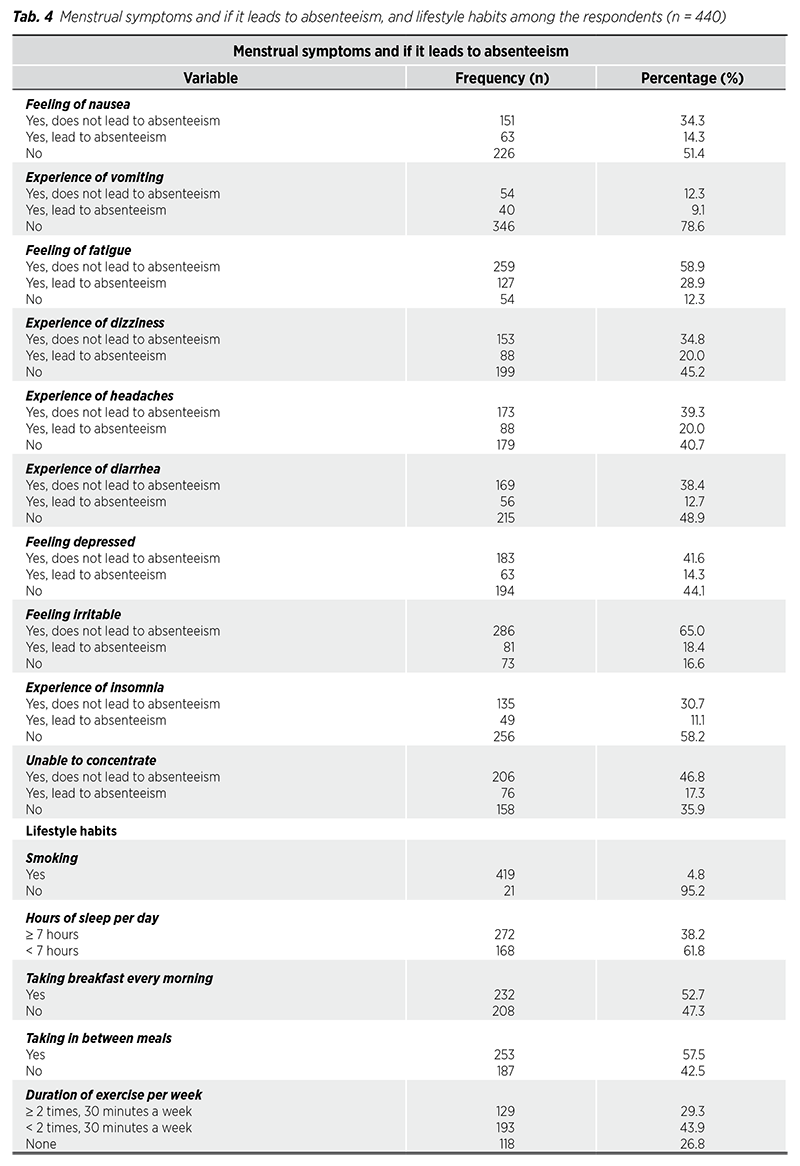
According to Table 4, menstrual symptoms significantly impacted absenteeism among women, with various symptoms leading to different rates of missed work or school days. For instance, feelings of nausea contributed to absenteeism in 14.3% of cases, while 34.3% reported no absenteeism due to this symptom. Vomiting led to absenteeism in 9.1% of cases, with 12.3% not experiencing absenteeism. Fatigue was a major factor, causing absenteeism in 28.9% of cases and not affecting 58.9%. Dizziness and headaches each led to absenteeism in 20.0% of cases, while not affecting 34.8% and 39.3%, respectively. Diarrhea resulted in absenteeism for 12.7%, with 38.4% unaffected, while feelings of depression and irritability led to absenteeism in 14.3% and 18.4% of cases, respectively, with non-absenteeism rates at 41.6% and 65.0%. Insomnia affected absenteeism in 11.1% of cases, with a nonabsenteeism rate of 30.7%, and the inability to concentrate led to absenteeism in 17.3%, affecting 46.8% who did not miss work or school.
In terms of lifestyle habits among a total of 440 respondents, a vast majority (95.2%) reported they did not smoke, while only a small percentage (4.8%) were smokers. Sleep patterns indicated that 61.8% slept less than seven hours per day, whereas 38.2% achieved at least seven hours of sleep nightly. Breakfast consumption showed that slightly over half (52.7%) ate breakfast daily, while nearly half (47.3%) skipped it. Snacking between meals was common, with 57.5% engaging in this behaviour compared to 42.5% who did not snack at all. Exercise frequency revealed that only 29.3% met the recommended guideline of exercising at least twice a week for thirty minutes; conversely, 43.9% exercised less than this amount, and 26.8% reported no exercise activity whatsoever.
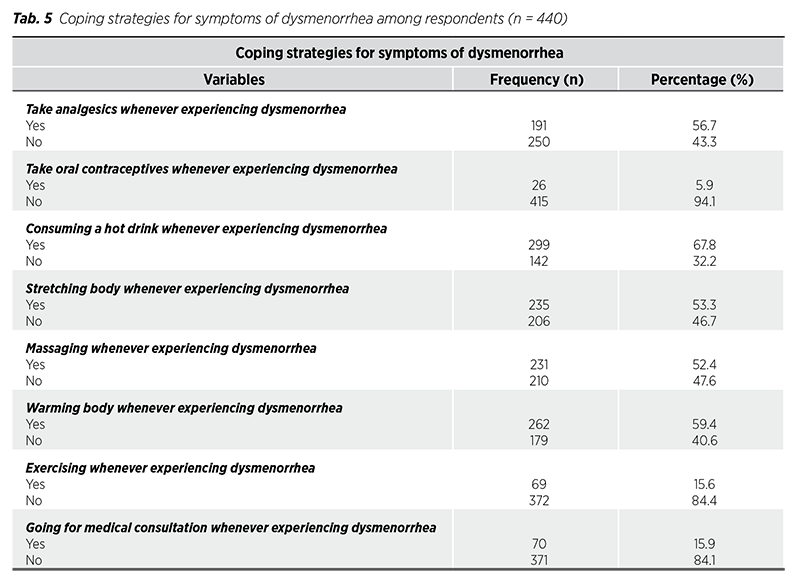
Table 5 listed numerous coping strategies for dealing with dysmenorrhea symptoms in a population. 56.7% of people took analgesics to treat pain, whereas 43.3% did not. Oral contraception was infrequently used as a treatment option, with only 5.9% reporting use and 94.1% avoiding it. During dysmenorrhea, the majority (67.8%) preferred hot liquids, while 53.3% stretched their bodies to relieve discomfort. Similarly, 52.4% used massage therapy to relieve discomfort, and 59.4% used body-warming techniques. However, just 15.6% exercised as a coping mechanism, whereas a huge majority (84.4%) avoided physical activity. This data showed that, while most people relied on easy self-care measures like hot drinks, stretching, and warming techniques, the usage of medicine and professional medical aid was quite low, with physical activity being the least popular means of dealing with dysmenorrhea. In short, this data proved that there was significant variation in the coping mechanisms used for the management of dysmenorrhea among females aged 18 to 50 years old in Malaysia, which rejected the null hypothesis that stated there was no significant variation in the coping mechanisms used.
Figure 2 Pie chart showed numerous coping strategies women used to treat discomfort due to menstrual cramps. Going to the medical consultation was the most favoured approach, with 67.8% of respondents, followed by do a massage (59.4%) and consuming hot drink (53.3%) for their body. Stretching the body were a popular alternative, with 52.4% choosing this method. The use of analgesics (56.7%), exercise (15.8%), and warming the body (15.9%) were the less favoured approaches. Oral contraceptives were the least used method, accounting for only 5.9%. The pie chart indicated women preferred non-pharmacological therapies such as hot liquids, body warming, and stretching, compared to using medical interventions such as analgesics, seeking medical counsel, or using oral contraceptive pills.
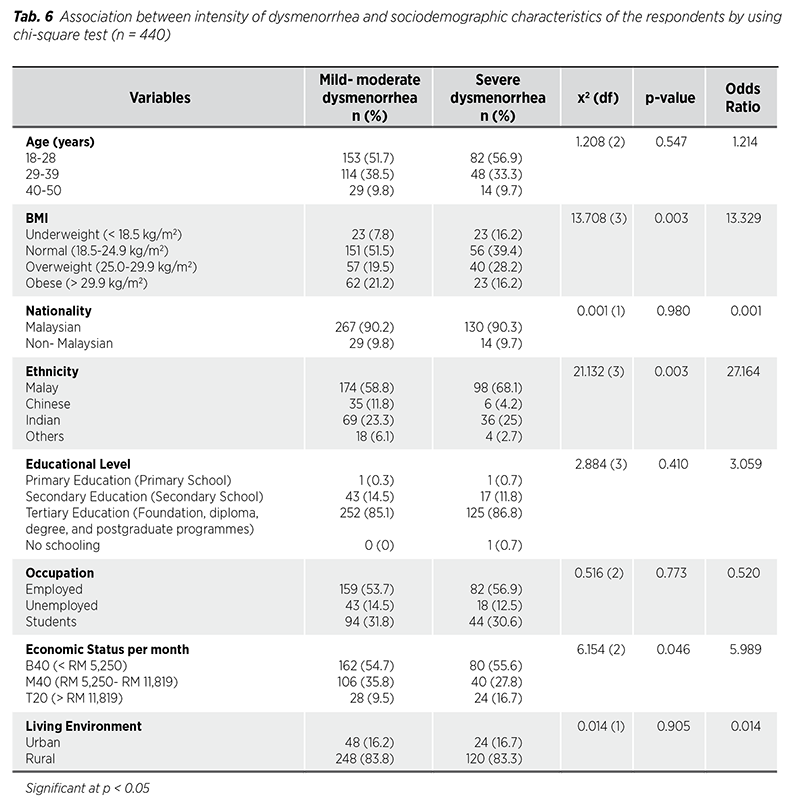
According to Table 6, there were no significant associations between age and intensity of dysmenorrhea (p = 0.547), while Body Mass Index (BMI) had a strong association with the severity of dysmenorrhea. Higher BMI was linked to increased dysmenorrhea severity (p = 0.003, OR 13.329). Nationality and living environment had no significant effect on the severity of dysmenorrhea (p = 0.980 and p = 0.905, respectively). Ethnicity, particularly with Malays reporting the highest severity (p = 0.003, OR 27.164). Educational level and occupation showed no significant associations (p = 0.410 and p = 0.773). Economic status indicated that lower economic groups (B40) experienced more severe dysmenorrhea (p = 0.046, OR 5.989).
Table 7 discussed the association between the intensity of dysmenorrhea and various characteristics, including situations that triggered or intensified menstrual pain. The duration of pain test revealed no significant difference between mild-moderate and severe dysmenorrhea groups (p = 0.329), although severe dysmenorrhea had a higher odds ratio (5.701) for lasting longer. The chi-square test for menstrual discomfort showed a significant difference (p < 0.001) between groups, with an odds ratio of 18.324 indicating those with mild-to-moderate dysmenorrhea were more likely to report higher discomfort levels. The degree of dysmenorrhea correlated significantly with a family history of the condition (p < 0.001). The odds ratio of 18.268 suggested individuals with a family history were significantly more likely to suffer from severe dysmenorrhea than those without. There was no discernible variation in the rhythmicity of the monthly cycle (normal, polymenorrhea, menorrhagia) between mild-moderate and severe dysmenorrhea (p = 0.389). A slight non-significant tendency for severe dysmenorrhea to link to aberrant cycle rhythmicity was indicated by the odds ratio of 1.820.
All situations (full bladder, urinating, bowel movement, walking, being seated, lifting weights) showed a highly significant association with severe dysmenorrhea (p < 0.001). The odds ratios were high, suggesting individuals with severe dysmenorrhea were much more likely to experience pain from these circumstances. There was no significant difference in pain experienced during sexual
activity between mild-moderate and severe dysmenorrhea (p = 0.238), although the odds ratio (4.108) indicated that individuals with severe dysmenorrhea may be somewhat more likely to experience pain during intercourse. This finding was not statistically significant, suggesting random variation. A strong link existed between dysmenorrhea intensity and pain experienced while walking (p < 0.001), with an odds ratio of 98.479 indicating individuals with severe dysmenorrhea were much more likely to feel pain while walking. Similarly, there was a significant difference in pain while seated (p < 0.001) and while lifting weights (p < 0.001), with odds ratios of 113.908 and 105.187, respectively, showing that severe dysmenorrhea strongly associated with increased pain during these activities.
The chi-square test results revealed significant associations between factors such as the amount of menstrual pain, family history, and specific pain-triggering situations with severe dysmenorrhea. However, duration of pain and menstrual cycle rhythmicity did not show statistically significant differences between the severity groups. These findings suggested that family history and external triggers played crucial roles in the intensity of dysmenorrhea. Table 7 also examined how dysmenorrhea affected various life aspects. Individuals with severe dysmenorrhea reported a much higher degree of disruption in their daily routines than those with milder symptoms. The odds ratio of 73.039 indicated that individuals suffering from severe dysmenorrhea were more than 70 times more likely to experience disruptions, with a p-value under 0.001 confirming this statistically significant difference. This showed severe dysmenorrhea could greatly diminish a person‘s ability to carry out daily tasks.
The ability to stay focused in class was heavily compromised for those with severe dysmenorrhea. Individuals with severe dysmenorrhea were 45.279 times more likely to experience attention problems during class than those with
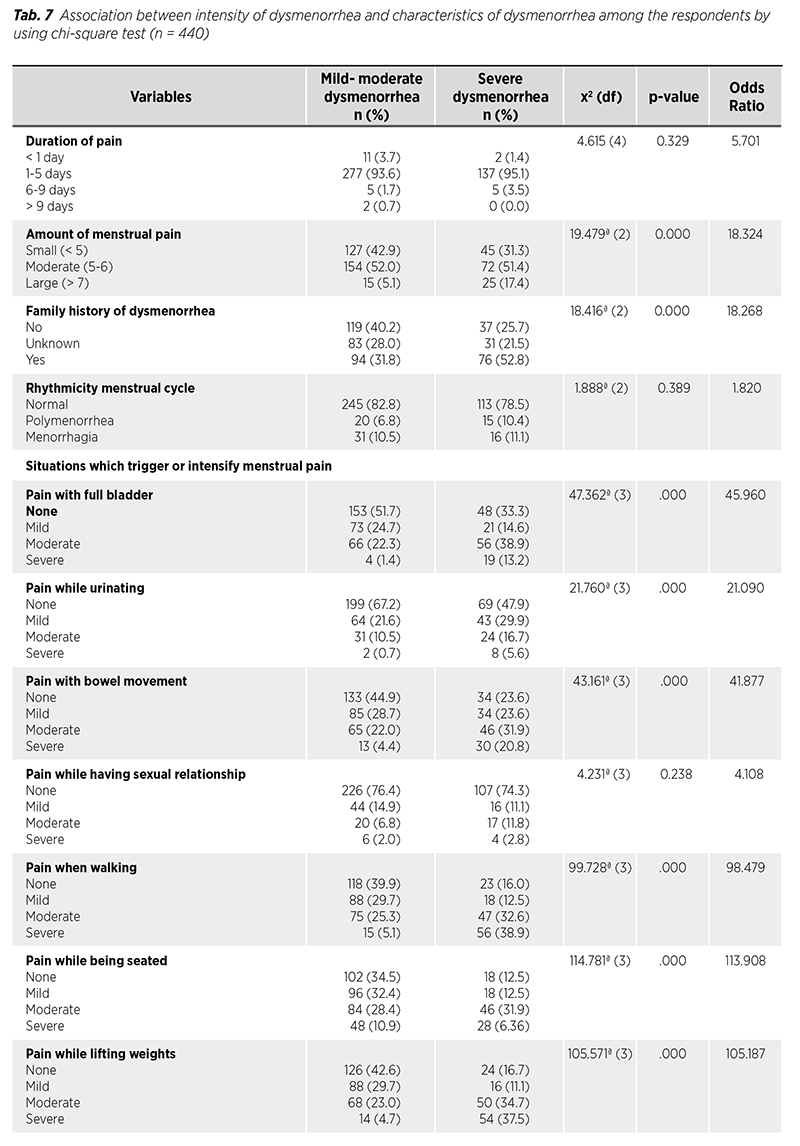
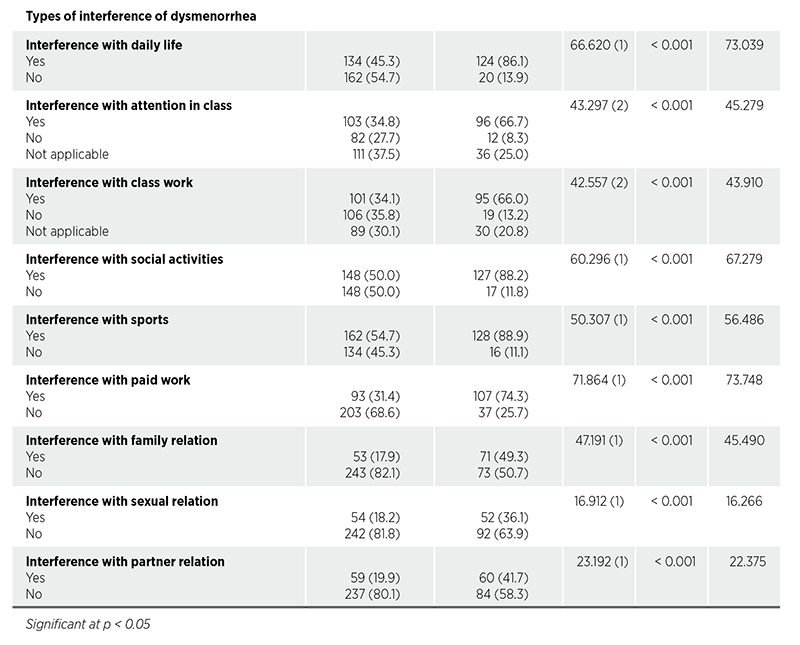
milder symptoms, supported by a p-value below 0.001. These findings suggested that dysmenorrhea significantly impacted academic performance, potentially leading to issues like poor grades or increased absenteeism.
In terms of classwork interference, 34.1% of those with mild to moderate dysmenorrhea reported issues, while 66.0% of individuals with severe dysmenorrhea did, with a chi-square value of 42.557 and a p-value of less than 0.001 indicating a statistically significant association. Similarly, severe dysmenorrhea significantly affected work performance, with p-values below 0.001 and an odds ratio of 73.748, suggesting that individuals with severe dysmenorrhea were over five times more likely to report difficulties at work. Dysmenorrhea also impacted social activities and sports participation. Individuals with severe dysmenorrhea were much more likely to experience interference in social events (OR 67.279) and sports (OR 56.486), with p-values below 0.001. Additionally, family and sexual relationships were notably affected, with individuals with severe dysmenorrhea being 45.490 times more likely to face family relationship difficulties and 16.266 times more likely to experience interference in their sexual relationships. Lastly, regarding partner relationships, among those with mild to moderate dysmenorrhea, 19.9% reported interference, while 41.7% of those with severe dysmenorrhea did. The chi-square value of 23.192 with a p-value less than 0.001 indicated a statistically significant association.
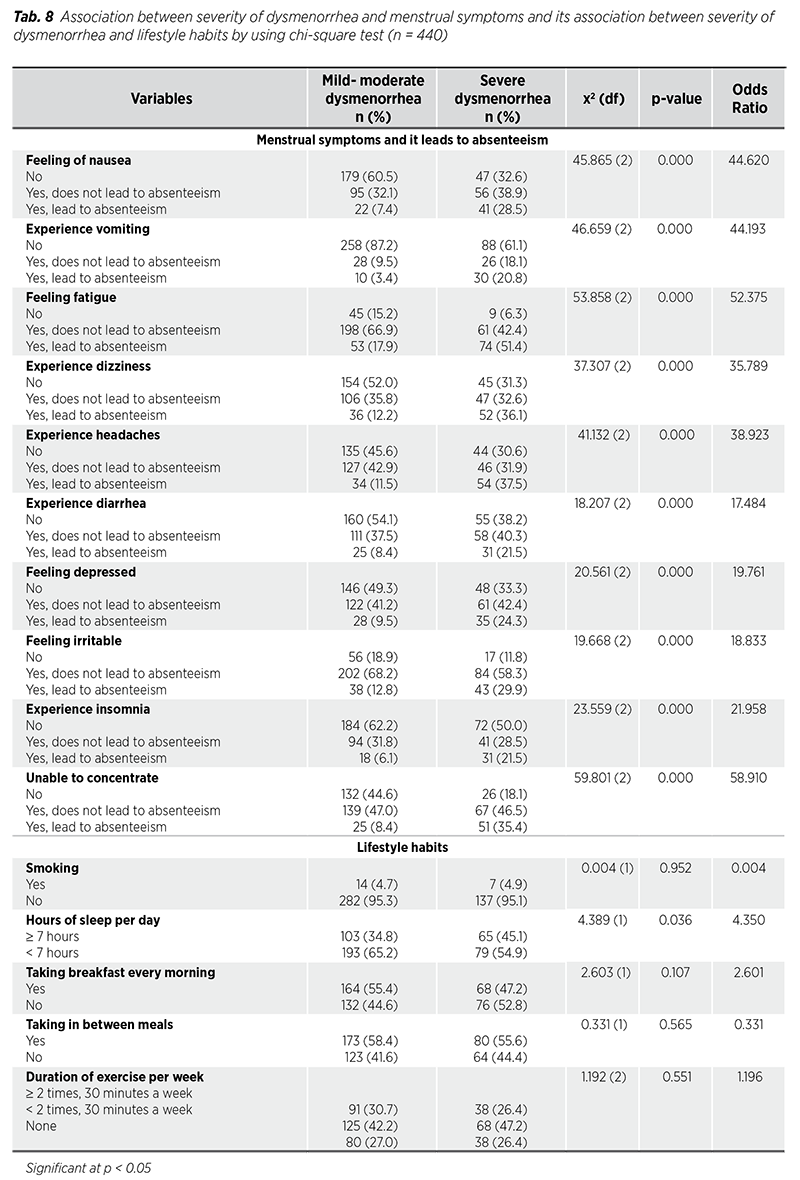
Based on the Chi-square test results, severe dysmenorrhea significantly correlates with absenteeism due to various symptoms, as evidenced by a series of statistical analyses. Nausea and vomiting show particularly high absenteeism rates, with 28.5% and 20.8% of those experiencing severe dysmenorrhea absent from work, compared to 7.4% and 3.4% in mild-moderate cases, respectively (p = 0.000, x2 = 45.865 and p = 0.000, x2 = 46.659). Fatigue is another major factor, affecting 51.4% of severely affected individuals versus 17.9% in milder cases (p = 0.000, x2 = 53.858). Dizziness and headaches also demonstrate significant absenteeism rates of 36.1% and 37.5%, respectively, among those with severe dysmenorrhea (p = 0.000 for both). Other symptoms such as diarrhea (21.5%), depression (24.3%), irritability (29.9%), insomnia (21.5%), and inability to concentrate (35.4%) further contribute to absenteeism, all showing significant statistical associations (p = 0.000). Conversely, lifestyle factors like smoking, breakfast consumption, meal frequency, and exercise frequency do not show significant relationships with absenteeism, although sleep duration does correlate significantly with absenteeism among those with severe dysmenorrhea (p = 0.036).
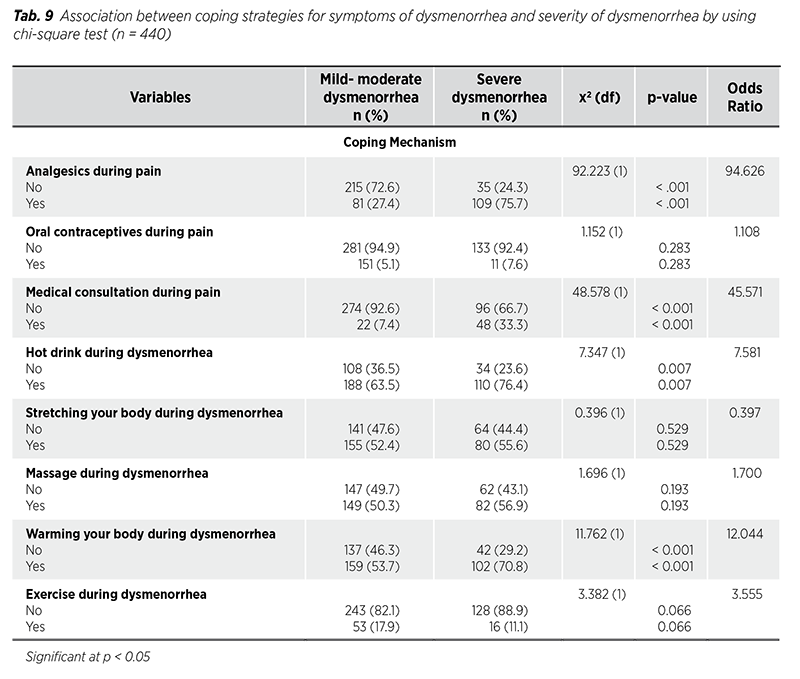
Analgesic use among women with mild to moderate dysmenorrhea showed that 215 (72.6%) did not use analgesics, while 81 (27.4%) did. In severe cases, 35 (24.3%) did not use analgesics, compared to 109 (75.7%) who did. The chi-square value of x2 = 92.223 and a p-value of < 0.001 indicate a strong reliance on pain relief medications in severe cases. Regarding the use of oral contraceptives, 281 (94.9%) of those with mild to moderate dysmenorrhea did not use them, compared to 133 (92.4%) in the severe group. The chi-square value of x2 = 1.152 and p = 0.283 show no statistical significance. Additionally, 96 (66.7%) women with severe dysmenorrhea did not consult a doctor, compared to 274 (92.6%) in the mild to moderate group. This resulted in a chi-square value of x2 = 48.578 and p < 0.001, highlighting an increased need for professional help in severe cases. In terms of hot drink consumption, 34 (23.6%) with severe dysmenorrhea did not consume hot drinks, compared to 188 (63.5%) in the mild to moderate cases, supported by x2 = 7.347 and p = 0.007. Stretching showed no significant difference between groups (x2 = 0.396, p = 0.529), and massage usage also did not differ significantly (x2 = 1.696, p = 0.193). A significant increase in warming techniques was observed, with only 42 (29.2%) of those with severe dysmenorrhea not using them, compared to 137 (46.3%) in the mild to moderate group (x2 = 11.762, p < 0.001). Finally, there was less duration of exercise among women with severe dysmenorrhea, as 128 (88.9%) did not exercise; however, this did not show statistical significance (x2 = 3.382, p = 0.066).
This study aimed to investigate the socio-demographic characteristics of respondents of Malaysia regarding the prevalence and impact of dysmenorrhea, specifically among females aged 18 to 50 years. Initially, 474 participants were recruited, of whom 61.8% identified as Malay. Although estimating the prevalence of dysmenorrhea in this population proved challenging due to non-probability convenience sampling, the findings suggested a significant prevalence rate of around 93%. Among the respondents, 43% experienced moderate dysmenorrhea, 30.4% reported severe dysmenorrhea, 19.4% had mild symptoms, and 7.2% did not experience dysmenorrhea at all.
The study revealed that severe dysmenorrhea was most common among women aged 18-28, with a prevalence of 56.9%. In comparison, 33.3% of the 29-39 age group reported severe symptoms, while only 9.7% were in the 40-50 age group. Although younger women reported higher rates of mild to moderate dysmenorrhea, a chi-square test (x² = 1.208, p = 0.547) showed no significant correlation between age and the severity of dysmenorrhea, suggesting that age did not substantially influence the likelihood of experiencing severe symptoms. However, existing literature, including a study by Philip et al. (2016), indicated that dysmenorrhea is more prevalent among younger females, as younger women, especially those in their late teens and early twenties, typically experience higher levels of hormonal fluctuations during their reproductive years. Prostaglandins, hormone-like substances that trigger uterine contractions, are often produced in greater quantities during menstruation in younger women (12).
The relationship between the severity of dysmenorrhea and various socio-demographic factors such as age and body mass index (BMI) was analysed using a chi-square test. No significant association was observed between age groups and dysmenorrhea intensity (p = 0.547). However, a significant association was found between BMI and dysmenorrhea severity (p = 0.003), suggesting that overweight or obese women were more likely to experience severe dysmenorrhea. This finding aligns with existing literature that associates higher BMI with increased inflammatory markers, which may contribute to more severe menstrual pain. The odds ratio of 13.329 indicated that being overweight or obese significantly increased the likelihood of severe dysmenorrhea. Furthermore, previous literatures noted that lower BMI among younger females correlated with higher dysmenorrhea severity and prevalence, suggesting a greater risk for younger women (13,14).
Ethnicity demonstrated a significant correlation (p = 0.003, OR 27.164), indicating that Malay women reported higher severity of dysmenorrhea compared to women of other ethnicities. Several factors could explain this increased prevalence among Malay women. Cultural, genetic, or lifestyle differences might contribute to this outcome. For instance, socio-cultural practices, dietary habits, or genetic predispositions unique to the Malay population might influence the severity and experience of dysmenorrhea. Additionally, other factors like health-seeking behaviour, access to healthcare, or awareness about dysmenorrhea could play a role in how symptoms were perceived and reported. According to Rana Mohamad Bakro et al. (2023), about 50% of those experiencing severe dysmenorrhea were Malays (4). Economic status also showed a significant correlation (p = 0.046, OR 5.989), suggesting that women in the T20 income category reported more severe dysmenorrhea. No significant differences were noted in educational level (p = 0.410, OR 3.059), occupation (p = 0.773, OR 0.520), or living environment (p = 0.905, OR 0.014), and nationality showed no significant difference in severity (p = 0.980, OR 0.001) (15).
The study also examined the association between characteristics of dysmenorrhea and severity. The duration of pain showed no significant association (p = 0.329) with dysmenorrhea severity. However, the intensity of menstrual pain was strongly associated with dysmenorrhea severity (p < 0.001), shown that those with higher pain scores (> 7) were more likely to report severe dysmenorrhea. According to the previous studies, there was a significant association between young age (18-24 years) and severity of dysmenorrhea (6,7). However, those findings were contrary with the findings from our study in which age factors had no significant association with severity of dysmenorrhea with p-value of 0.329 (> 0.05). A family history of dysmenorrhea also played a crucial role (p < 0.001), where individuals with a family history were more likely to experience severe dysmenorrhea, suggesting a possible genetic predisposition. Ju et al. (2014) reported that a family history of dysmenorrhea strongly increased its risk, with odds ratios ranging between 3.8 and 20.7. Additionally, situational factors such as pain related to a full bladder, bowel movements, or walking were significantly associated with severe dysmenorrhea (p < 0.001), underscoring the exacerbating effects of these situations on pain perception (16).
The study found that dysmenorrhea severely disrupted daily life. Individuals with severe dysmenorrhea were over 70 times more likely to experience interruptions in their routines compared to those with mild to moderate symptoms, a statistically significant finding (p < 0.001). Students with severe dysmenorrhea struggled significantly to maintain focus in class, reflected by an odds ratio of 45.279, along with strong statistical support. Additionally, 66% of those with severe symptoms reported interference with classwork, compared to only 34.1% of those with milder symptoms, supported by an odds ratio of 43.910. In the workplace, individuals with severe dysmenorrhea were over five times as likely to face difficulties, negatively impacting their productivity. The condition also limited participation in social and sports activities, with odds ratios of 67.279 and 56.486, respectively, both statistically significant (17).
Interpersonal relationships were similarly affected, with a 45.490 times greater likelihood of issues in family relationships and a 16.266 times greater likelihood of challenges in sexual relationships among those with severe dysmenorrhea. These findings were consistent with the findings from previous study done among Serbian university students indicated that 41.7% of individuals with severe dysmenorrhea experienced partner relationship interference, in contrast to 19.9% of those with milder symptoms, highlighting a significant impact (OR 22.375) (17). Overall, a clear and statistically significant association was observed between the severity of dysmenorrhea and its detrimental effects on multiple facets of life (17-19).
Additionally, the study explored the relationship between dysmenorrhea severity, menstrual symptoms, and absenteeism. A significant relationship was noted between symptoms like nausea, vomiting, and fatigue with absenteeism, particularly in cases of severe dysmenorrhea (p < 0.001). Women experiencing vomiting or fatigue were more likely to miss activities due to their symptoms, suggesting a heightened burden of dysmenorrhea on daily functioning. Philip et al. (2016) indicated that dysmenorrhea negatively affected quality of life, with symptoms such as mood fluctuations, reduced academic performance, and strained relationships reported by respondents (12). Durand et al. (2021) also supported the notion that dysmenorrhea adversely impacts quality of life, stating that pain catastrophizing significantly predicted both pain intensity and interference with daily activities (20).
Lifestyle habits had a limited association with the intensity of dysmenorrhea. For instance, smoking and exercise showed no significant correlation with the severity of dysmenorrhea (p > 0.05). Ju et al. (2013) found inconclusive evidence regarding modifiable factors such as cigarette smoking, diet, obesity, depression, and abuse. However, sleep duration was significant (p = 0.036), as individuals sleeping less than seven hours a day were more likely to report severe dysmenorrhea, suggesting that sleep quality may influence pain perception or recovery (16).
The study also analysed coping strategies utilized by women suffering from dysmenorrhea and their effectiveness concerning pain intensity. The use of analgesics showed a strong association with severe dysmenorrhea (p < 0.001), with many women experiencing severe pain using analgesics during their periods. Medical consultation was common among women with severe dysmenorrhea (p < 0.001), indicated that individuals with more intense pain were more likely to seek professional help. Non-pharmacological methods, such as warming the body during dysmenorrhea (p < 0.001), were frequently employed by those experiencing severe symptoms. This suggests that individuals facing higher pain intensity often resort to multiple coping mechanisms, including medical interventions and self-care strategies, to alleviate symptoms. These findings were consistent with the findings by Durand et al. (2021) indicated that non-pharmacological strategies, such as heat application (79%) and rest (60.4%), were commonly favoured, with analgesics being used by 79.5% of participants, primarily paracetamol (60.5%), despite its limited effectiveness (20,21). Moreover, there were some effective strategies to improve dysmenorrhea symptoms such as regular exercises, dietary adjustments by increasing the intake of low-fat foods to reduce menstrual pain, and some alternative strategies were suggested by previous literatures (9). For instances, psychological and stress management therapy such as cognitive behavioural therapy (CBT) and stress reduction therapy were also effective. Furthermore, some literatures suggested that by providing comprehensive menstrual health education and fostering open discussion in school and communities could empower individuals to manage their symptoms more effectively (3,10).
In analysing the results, a few unexpected and expected findings emerged during the research. Notably, regarding age, there was one participant aged 11 and three participants over 50, which fell outside the target demographic of 18 to 50 years. Furthermore, the open-answer format for the age section led to some responses that did not align with the question. Additionally, despite targeting females, the study attracted some male participants, resulting in a final sample size reduction from 480 to 440 after screening out irrelevant responses.
Overall, the statistical analysis indicated significant findings regarding dysmenorrhea prevalence and its impact on daily activities among the study population. The prevalence rate of dysmenorrhea was determined to be 65%, reflecting the substantial burden of this condition. Findings indicated that females with dysmenorrhea significantly influenced daily activities such as work performance, social engagements, and physical activities compared to those without the disorder. Existing research literature supports these findings, revealing a significant rate of dysmenorrhea, although the level of impact on daily living varied due to geographical and cultural differences (15,22).
To conclude, this study shows that dysmenorrhea has a significant impact on the quality of life of most women experiencing moderate to severe pain lasting 1 to 3 days. Dysmenorrhea causes physical discomfort and affects daily activities such as walking, sitting, and social engagement. From the data collected, the presence of a family history was a notable factor as 31.8% of women who presented with mild to moderate symptoms of dysmenorrhea and 52.8% of women with severe dysmenorrhea have stated the same, most likely suggesting that there could be a genetic link. The menstrual pain was not limited to the pelvic area, as many individuals reported discomfort while walking, sitting, lifting weights, and during bowel movements, indicating that dysmenorrhea affects more than just the reproductive system. These findings highlight the need for interventions to alleviate pain and improve the daily functioning of life, particularly in areas like work, academics, and physical activities. Effective management strategies could greatly enhance the well-being of those affected by dysmenorrhea, thus reducing its overall burden for women. By using convenience sampling in our study, there was the potential for selection bias which can limit the generalizability of the findings, thereby introducing systematic differences that could skew the results. Therefore, future studies should consider employing probability sampling techniques to enhance the representativeness and generalizability of findings.
First of all, we would like to express our sincere gratitude and our appreciation towards all the willing participants of our study. And, we would also like to thanks the Research Ethics Committee, Faculty of Medicine, Manipal University College Malaysia for approving our research. Moreover, we would like to warmly express our appreciation towards Professor Dr. Adinegara Lutfi Abas (Pro Vice Chancellor of Manipal University College Malaysia), Professor Dr. Jayakumar Gurusamy (Dean of Faculty of Medicine, MUCM), supervisors and lecturers for providing their invaluable guidance, comments and suggestions throughout the course of the project.
There was no conflict of interest in this study.
There were no funding supports for this study.