









 Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.
Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.

Bowel evisceration is a rare but severe complication that can occur following gynecological surgeries. This report details the case of a 45-year-old woman who experienced bowel evisceration one year after undergoing a total laparoscopic hysterectomy with bilateral salpingectomy. The evisceration occurred spontaneously at the time of using the toilet for the purpose of emptying the stool. The patient had no prior surgical abdominal history and no identified risk factors such as recent sexual intercourse or vaginal examination. This case underscores the importance of meticulous vaginal cuff closure during any form of hysterectomy and highlights the unpredictable nature of delayed bowel evisceration.
Bowel evisceration is an uncommon but potentially life-threatening event that can follow abdominal and gynecological surgeries. Although more commonly is seen shortly after surgical procedures, delayed occurrence is rare and usually unexpected. There is limited amount of reported cases in current literature (1). Therefore, we present a unique case of spontaneous bowel evisceration occurring one year post-operatively in a patient with no predisposing risk factors. We would like to emphasize the necessity of early diagnosis in order to eliminate possible complications and the importance of a multidisciplinary approach in surgical therapy.
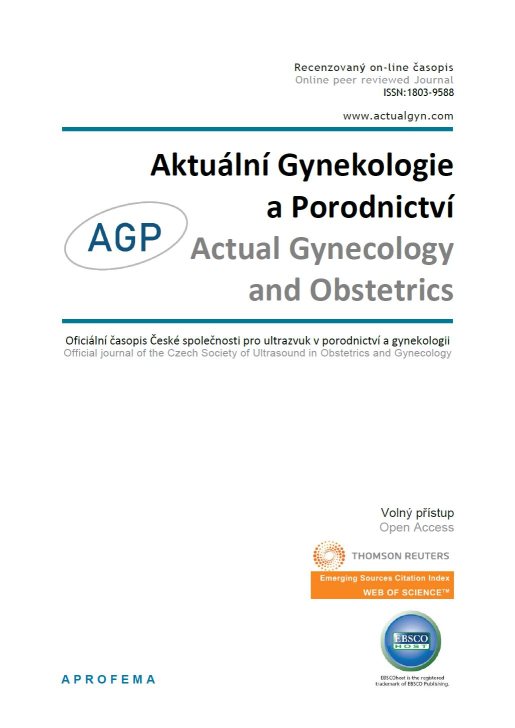
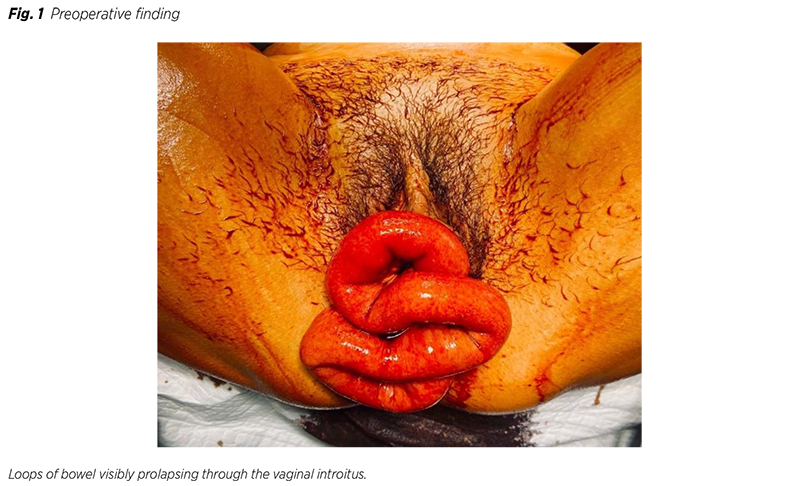
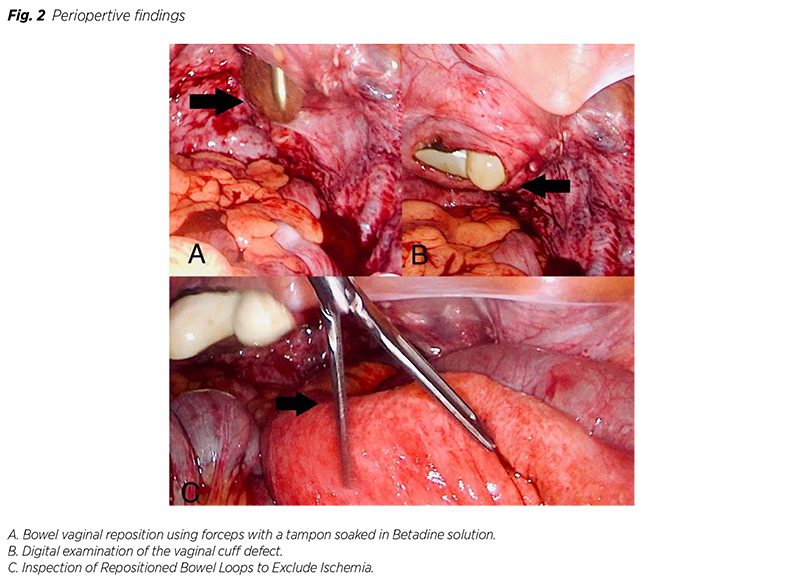
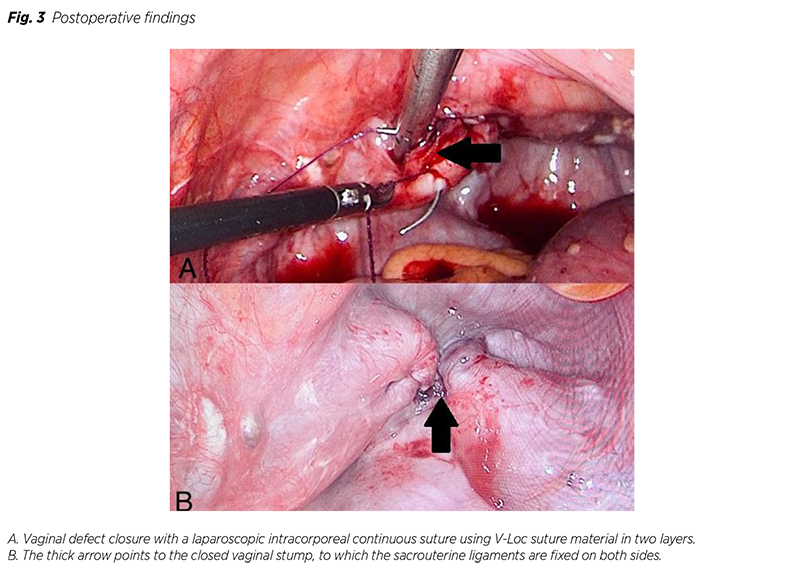
A 45-year-old woman, with no previous surgical history was presented to the emergency department with bowel evisceration occurring at the toilet usage. Firstly, she complained of feeling something falling out of her and palpation of mass in front of external genital. She underwent a total laparoscopic hysterectomy (TLH) with bilateral salpingectomy one year ago due to the uterine descens grade I in postmenopausal period, preterm menopause in 2015. Notably, there were no predisposing risk factors such as recent sexual intercourse or vaginal examination. The patient was initially transported by paramedics to the hospital, which was the closest and at the same time the center with the highest level of competence. Unfortunatelly, the hospital refused to perform surgery, they stated because of the primary surgery was not performed there. They ordered patient transport to our facility, despite their competence superiority or even initial examination. Upon arrival at the Gynecology and obstetrics department in our hospital, the patient was diagnosed with bowel evisceration, fatigue and dizziness. She was hypotensive and tachycardic. Due to the rapid development of neurogenic shock symptoms, she was promptly transferred to operating theatre for immediate surgical intervention and revision. During initial inspection and examination, loops of bowel were visibly protruding through the vaginal introitus (Fig. 1). The patient‘s CRP level was 120, indicating a significant inflammatory response She was quickly prepared for laparoscopic revision of the abdominal cavity and vaginal repositioning of the eviscerated bowel. The surgical team consisted of general surgeon and gynecologist as the best suggested multidisciplinary approach. Intraoperative findings included multiple loops of small intestine protruding through a defect in the vaginal cuff. The eviscerated bowel appeared viable with no evidence of ischemia or perforation. During the surgical procedure, the bowel was repositioned vaginally using tampon forceps with a tampon soaked in Betadine solution. Consequently, laparoscopic assistance with an intestinal grasper was provided due to the edematous nature of the bowel loops, which made gentle repositioning challenging. Following the repositioning, the surgeon laparoscopically evaluated the repositioned bowel loops to rule out ischemia. Fortunately, no ischemia was present; the bowel loops appeared pink and viable. The vaginal cuff defect measured 6 x 4 cm without bleeding (Fig. 2). The edges of the vaginal cuff were freshened using laparoscopic scissors, and the defect was closed with a laparoscopic intracorporeal continuous suture using V-Loc suture material in two layers (Fig. 3). The abdominal cavity was thoroughly irrigated, and no other intra-abdominal pathology was found. The total time from the onset of bowel evisceration to the beginning of the surgical procedure was approximately 230 minutes. She received a combination antibiotic therapy of amoxicillin/clavulanic acid (625 mg every 8 hours orally) and metronidazole (500 mg every 8 hours orally). She was closely monitored postoperatively on ICU and her recovery was uneventful. She reported no pain, and her inflammatory markers decreased significantly, with CRP levels dropping from 120 to 45 after 48 hours. Monitoring of CRP levels was crucial to uncover possible infection or complications. She was discharged home on the fourth postoperative day with instructions for restricted activity and close out patient follow-up. At her six-week postoperative visit, she reported no further complications and was resuming normal activities.
Bowel evisceration through the vaginal cuff is a rare but serious complication following vaginal surgeries including different techniques of hysterectomy (2,3). It was firstly described in 1864 and till now there is only approximatelly hundred reported cases (90 articles on Pubmed since 1994) (1). It is characterized by the separation of the vaginal vault and presents a significant risk of pelvic contents, particularly the small bowel, protruding into the vagina (4). It typically occurs within weeks to months postoperatively, often associated with precipitating factors such as sexual activity, vaginal examination, radiotherapy, vaginal atrophy, increased intra-abdominal pressure, intermittent abdominal pain, bloating, and chronic constipation (2,5,6). This case is unique due to the delayed onset and absence of these risk factors. The exact mechanism of delayed evisceration
in this patient remains unclear but may relate to incomplete healing or chronic strain on the vaginal cuff. Secure vaginal cuff closure is critical to prevent this complication (7). Although the literature presents case reports in which different surgical techniques were used at different time periods after primary surgery, the conclusions and recommendations are the same in the most cases. They highlight the importance of secure vaginal cuff closure to prevent such complications. Surgical treatment can be transabdominal, transvaginal or both based largely on the expertise available and the clinical situation of the patient. According literature review transvaginal approach is generally believed to be the least morbid, but in general it depends on individual case, approach and characteristics of the tissue itself (8). Techniques such as laparoscopic suturing, use of barbed sutures, and robotic-assisted suturing have been proposed to enhance cuff integrity (4,9,10). Prompt diagnosis and surgical intervention are crucial to prevent further complications, such as bowel ischemia or infection (10). Additionally, some studies suggest routine postoperative counseling regarding the avoidance of high-risk activities during the healing period (4,11).
Bowel evisceration after TLH is a rare but life-threatening complication. The absence of common risk factors in this case, such as recent sexual activity or vaginal examination, underscores the unpredictable nature of this condition. Future studies should explore patient-specific risk factors and surgical techniques to identify strategies for reducing the risk of delayed bowel evisceration. In this case, the laparoscopic approach allowed for thorough evaluation and effective management of the eviscerated bowel and the vaginal cuff defect. The successful outcome highlights the importance of a multidisciplinary approach, involving both gynecologic and general surgeons, in managing such complex cases.
Zuzana Ballová, MD, Tomáš Vasilenko, MD, Petra Gašparová, MD and Assoc. Prof. Erik Dosedla, MD, Ph.D., MBA have no conflicts of interest or financial ties to disclose. Written consent for publication of the article with photographic documentation without mentioning the patient‘s identity was obtained.