









 Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.
Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.

Discussion: Myofascial trigger points have become an area of considerable interest. In this brief note, we discuss pathophysiology, diagnostics and treatment. We highlight potential hindrances concerning the interpretation, duration and chronicity of pain.
The prevalence of chronic pelvic pain syndrome (CPPS) in women is quite high. Several patterns are helping to improve its understanding. However, the easiest division is based on the reason and source of pain, which could help determine the best treatment solution. Organic pain accompanies a particular disease and is mainly resolved by solving the underlying disorder. Pain originating from unknown, Inapparent causes is rarely resolved or effectively treated.
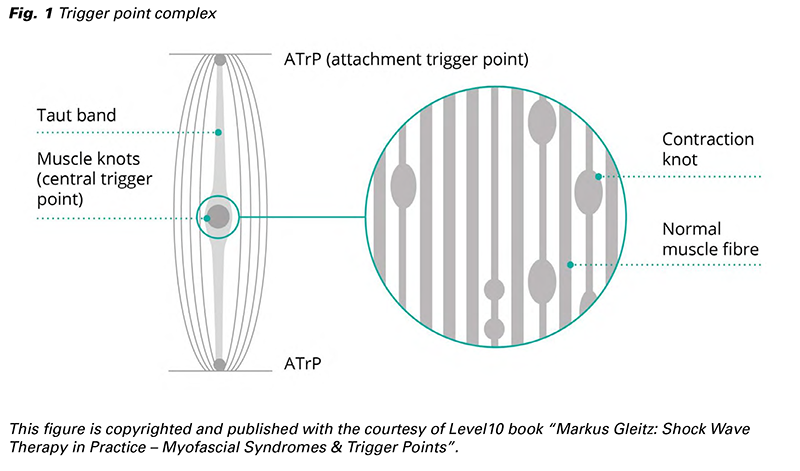
Large number of pains are associated with myofascial pain syndrome (MPS) (1-3). Within specific databases, the representation of MPS amounts to 10% of the total population. Many authors attribute it to myofascial trigger points (MTrPs, TrPs, i.e., tender, painful contraction knots) localized in the myofascial perineal area (Fig. 1). TrPs are a distinct form of ischaemic, localized muscle pain that can significantly impact the overall well-being of women. They are often linked to a referred pain, shifting the feeling of pain to the distant area. TrPs and normal muscle pain have similar pain mechanisms but differ in intensity, duration and healing ability. While typical muscle pain tends to resolve on its own, TrPs possess autonomous qualities and lack sufficient self-healing capacity. They often experience the progression of pain into a chronic state (2,4-8).
Arthur Steindler adopted the trigger point term (Bone Surgery, 1940) (9). The terms musculoskeletal trigger point, muscular scar, myogelosis and muscular hardening were coined by Janet Travell (Jama, 1942) (10).
Trigger points manifest as palpable nodules within the elongated bands of skeletal muscles, representing hyperirritable spots. TrPs originate from local muscle lesions causing neuromuscular endplate dysfunction. Compression of these structures can elicit pain, referred pain, tenderness, muscular dysfunction and vegetative phenomena (11-13).
Trigger points are generally divided into active and latent (chronic), according to their clinical status. A trigger point in an active state produces pain upon palpation or referred pain that is relocated to a region far from the primary nodule. A latent TrP does not result in pain upon palpation, but it does have a negative impact on the activity and functionality of the affected muscle. By applying firm pressure, it is possible to induce muscle twitching.
The presence of trigger points (TrPs) is exclusive to skeletal muscles, owing to their function and position within dynamic and postural range. The pelvic floor muscles, in particular, hold significant importance. Referred pain with roots in striated muscles could also affect smooth muscle organs. The explanation is based on the principle of Head’s zones. A contrary direction is also possible but without TrPs. Pelvic floor pain, often combined with organ dysfunction, should not be overlooked in this context (1,3,14,15).
Persistent local sarcomere contractions result in painful muscle knots from extensive nociceptor activity. This mechanism is adherent to a local energy crisis and endplate dysfunction. Different traumas (e.g., contusions, strains and sprains) could induce TrPs. It could be initiated by repetitive injuries, overloading and overuse of muscles, leading to chronic TrPs. Small muscle fibres type I, sometimes called Cinderella fibers, play an important role in creating MTrPs if injured. Studies on MTrPs reported a high frequency of spontaneous electrical potentials (SEAs) and contracture knots in the skeletal muscles of humans and animals. Speculation suggested that the neuromuscular junction exhibited an abnormal increase in acetylcholine (ACh) secretion, resulting in TrP development. Local TrPs were generated in trial by injection of an anti-acetylcholine esterase into a local normal muscle. Based on this premise, the theory of an additional release of ACh at the nerve endings in motor endplates was proposed. It describes an excessive release of ACh in the synaptic cleft, triggering high-frequency miniature endplate potentials and thus permanent depolarization. It prompts the sarcoplasmic reticulum to release large amounts of calcium. These processes result in the long-term contraction of clusters of muscle fibres and an elevation in muscle tone due to continual reduction in the length of the sarcomeres. Endplate dysfunction results in the permanent contraction of actin-myosin filaments. Because this contracture is limited to the area below the affected endplate, initiating any action potential is prevented. Therefore, the surface EMG does not reveal any changes. The main reasons for persistent contractures and nociceptor activity are local hypoxia and ischaemia (1,4,6,12,16).
Apart from the formation of contraction knots, the remaining parts of the muscle fibres are stretched passively and produce taut bands in the direction of the muscle fibre. The contraction of knots leads to the compression of vascular capillaries, resulting in local ischaemia. The muscle fibers at the nerve endings become cramped, with increasing local metabolic requirements.
Both ischaemia-induced energy deficiency and increased energy consumption for Ca-pump activation necessary for actin-myosin separation can contribute to developing a local energy crisis. The TrP is transferred under a condition similar to local rigour mortis. Muscular oximetry presents a significant decrease in oxygen in the location of myogenesis.
Meanwhile, the concentrations of histamine, serotonin, bradykinin, and substance P increase around the knots, and the local ischaemia worsens with swelling. It also sensitizes the afferent nerves. These events give rise to pain and the manifestation of local sympathetic symptoms. The process of vasoconstriction leads to a sensation of local coldness and alterations in central stress levels. Increased levels of sensitizing substances are found near trigger points.
Individuals who engage in minimal physical activity daily but experience occasional intense physical exertion are likelier to have trigger points. Individuals who engage in regular muscle exertion exhibit a decreased susceptibility to the disorder. Muscles frequently impacted by trigger points include the postural muscles and those in the shoulder and pelvic girdle (5,11,17).
The diagnosis of TrPs is primarily conducted through the palpation technique, which involves two prevalent approaches: Flat and Pincer. When employing the Flat palpation technique, which consists of applying fingers against deeper tissue layers, the recommended pressure range is 2-6 kg (Fig. 2). In the Pincer palpation technique, the particular muscle is palpated between the examiner’s fingers (Fig. 3). Once the taut band is identified, the move-along technique helps locate a highly sensitive and tense area including the muscle hardening. Muscle jump and local twitch response are present in accordance with expectations. Transferred pain could be evaluated the same way (3,9,10).


Laboratory techniques, such as direct muscle needle electromyography (EMG), may not always be accessible or preferred by the patient. Low potentials are characterised by an amplitude ranging from 10 to 80 μV, whereas high potentials have an amplitude ranging from 100 to 600 μV. Using basic surface EMG normally yields unsatisfactory outcomes (4,5,14,16).
Ultrasonography (US) shows promise as a viable approach now and possibly in the future. A promising technique is the implementation of colour flow mapping to depict the stiffness and compression within a specific area. Elastography represents an additional potential tool. A thorough investigation of the TrPs area may provide pertinent solutions. We understand that tangible trigger points are formed due to the accumulation of multiple trigger knots rather than a single one. Edematous swelling additionally assists in delineating an affected area (1,11,16,18-20).
The main principle is removing TrPs from their area or stopping their influence, which acts similarly. The self-healing capability of affected muscles is minimal (4,21).
The technique that received the highest recommendation involves applying strong pressure to the TrPs area followed by muscle stretching. Myorelaxans, antiflogistics and analgetics support this process (13).
The same needles employed in acupuncture are used in this method, with a direct emphasis on targeting TrPs. Many patients find this method too painful to undergo repeatedly (22).
Several applications fall under this umbrella term, mainly the local application of particular drugs.
This procedure primarily involves the administration of anaesthetic agents or antiphlogistics. Its main objective is to ease pain and potentially initiate the healing process.
Botulinum toxin A (Botox) is a popular agens for alleviating pain, contractures and other indications. It is a neurotoxin that blocks ACh’s release from presynaptic cholinergic nerve endings. Some histologically supported animal studies reported complete relief of TrPs by this drug. Even the local long-term analgetic effects should be considered (23).
Many physical methods are used in this area, including electrotherapy, laser application, ultrasound techniques and magnetotherapy. Magnetotherapy appears to hold considerable promise, contingent upon the accessibility of appropriate equipment.
We also need to mention shockwave techniques using radial and focused equipment (24,25). This approach has expanded our arsenal (14,24,26,27).
The problems associated with TrPs are frequently declined in orthopaedic surgeries, but less often in other departments. Pelvic girdle changes in pregnancy are known but typically disappear after birth. Still, long-term pelvic pains are not linked to a particular organic disease, yet they have a profound effect on quality of life. Vulvodynia is an example of such a condition, and dyspareunia significantly affects a woman’s personal life in a distinct, yet crucial manner.
Certain diagnostics and treatment problems are caused by Extramuscular trigger points localized at the attachment area of tendons to bones. They are mainly caused by chronic muscle shortening at the insertion site.
The duration of TrPs could not always be estimated immediately. The process often requires repeated approaches to prevent redirection and transformation in the spinal cord.
There are several limitations and reasons for errors in treating myofascial pain. Mistakes frequently arise when the severity of pain is undervalued due to the absence of detectable structural abnormalities through imaging methodologies.
Furthermore, the expectation is that these pain syndromes are self-healing. However, addressing chronic pain necessitates a proactive approach. There is also the risk of chronification and central pattern, which heals with difficulties.
In conclusion, our aim was to provide a brief yet comprehensive overview of the onset of muscle pain in general and specifically in the pelvic and perineal girdle regions. We primarily directed our attention towards inconspicuous concerns related to TrPs. We also wanted to highlight the recent treatment modalities of shock wave therapy and Botox administration. We would like to invite readers to the discussion about further directions in the pain treatment of pelvic floor and girdle.