









 Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.
Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.

Objective: This study aims to translate, validate, and assess the reliability of the Turkish version of the Perception of Obstetric Violence in Students Questionnaire (PercOV-S Q) and describe disrespectful and abusive mistreatment during facility-based childbirth.
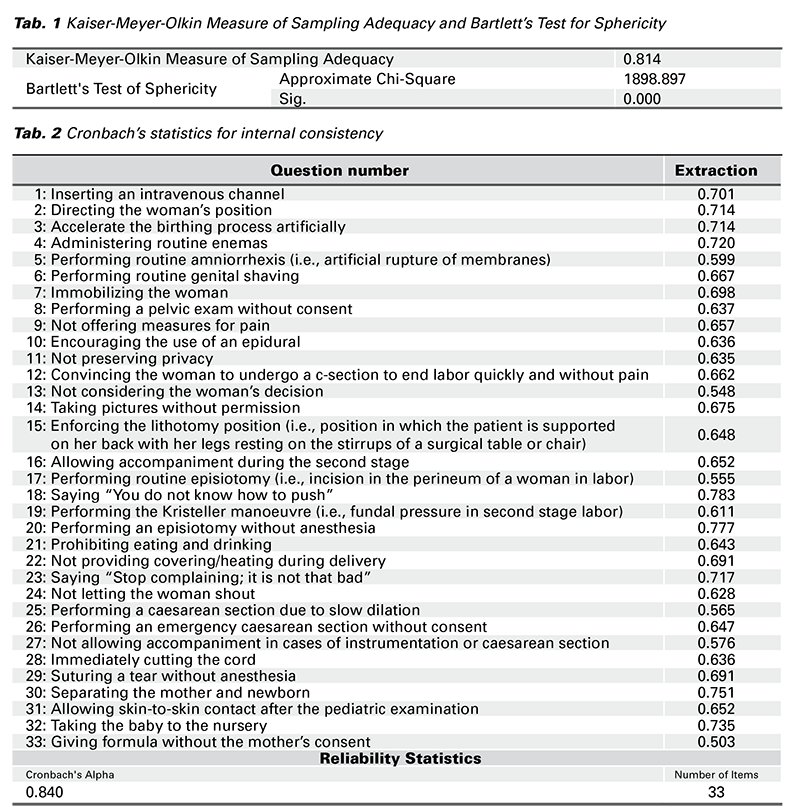
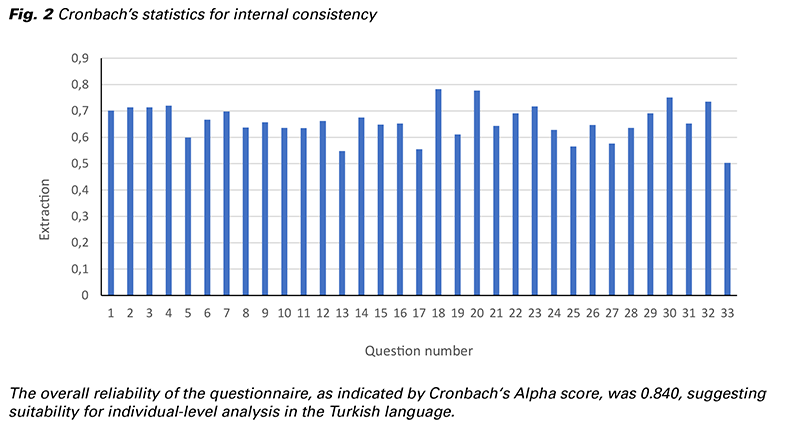
Materials and Methods: The PercOV-S Q, an objective questionnaire measuring perceived mistreatment during facility-based childbirth, comprising 33 positively worded questions on a 5-level Likert scale, was translated into Turkish. An online survey was sent to 140 obstetrics and gynecology residents via hospital email accounts, with 133 participants forming the cohort. Principal component factor analysis with varimax rotation was performed, and items with a loading of 0.40 on a principal components analysis were retained. The Cronbach's statistic was used to evaluate internal consistency, with a value of 0.70 indicating satisfactory internal consistency.
Results: The main result of this study is the Turkish translation of the PercOV-S Q is valid and reliable. The viability of factor analysis was confirmed by the Kaiser-Meyer-Olkin (KMO) test (p = 0.814) and Bartlett’s test for sphericity (X2 = 1898.897; p ≤ 0.001). The overall reliability of the questionnaire, measured by Cronbach's Alpha score, was 0.840, indicating the questionnaire is suitable at the individual level in Turkish.
Conclusion: The lack of a precise definition makes it difficult to understand the real perception among healthcare professionals and limits educational opportunities against obstetric mistreatment. In conclusion, the PercOV-S Q serves as a comprehensive and universal tool, and the Turkish translation of this questionnaire can be used as educational material. Translating and validating the PercOV-S Q across various languages and administering it to trainees from different cultural backgrounds will highlight its universal applicability and improve insights into the worldwide occurrence of obstetric mistreatment.
The World Health Organization (WHO) describes disrespectful and abusive treatment during childbirth in healthcare facilities as encompassing physical abuse, verbal humiliation, coercive or unauthorized medical procedures such as sterilization or episiotomy, breaches of confidentiality, failure to obtain full informed consent, refusal of pain medication, significant violations of privacy, denial of access to healthcare facilities, neglect of women during childbirth leading to life-threatening, preventable complications, and postpartum detainment of women and their newborns in facilities due to financial constraints. WHO underscores the absence of a global consensus on the scientific definition and measurement of disrespect and abuse, resulting in uncertainty regarding its prevalence and impact on women’s health, well-being, and decision-making (1).
While some South American countries, including Venezuela, Argentina, Brazil, and Mexico, have enacted legislation recognizing ‘obstetric violence’ (OV) as a violation of human rights, there remains considerable variation in their approaches. For instance, Venezuela pioneered legislative action in 2007, emphasizing women’s rights to a private life free from medical intervention that undermines autonomy and decision-making regarding their bodies and sexuality (2). Similarly, Argentina passed laws in 2009 recognizing OV as violence enacted upon women’s bodies and reproductive processes by healthcare professionals through dehumanizing practices and abuses in medication (3). In contrast, Brazilian legislation encompasses not only healthcare professionals but also family members or companions, broadening the scope of potential perpetrators (4). These divergent perspectives on obstetric mistreatment during facility-based childbirth underscore the challenge of identifying its true prevalence and impact within the healthcare community, thus representing a critical issue in public health and human rights discourse.
In 2015, the World Health Organization (WHO), along with several international organizations, developed the mother-baby friendly birthing facilities (MBFBF) initiative, setting clear criteria to combat obstetric mistreatment during facility-based childbirth (5). These criteria include ensuring privacy during labor and delivery, providing adequate pain relief, prohibiting various forms of abuse, and avoiding non-evidence-based practices such as routine episiotomy and separation of mother and baby care. In 2020, Mena-Tudela et al. developed and validated an objective questionnaire, based on the MBFBF criteria, for assessing perceived OV among nursing, midwifery, and medical students, available in both Spanish and English (6).
Obstetric mistreatment is a significant public and human rights issue that profoundly affects maternal care quality and women’s well-being globally. Building upon this work, our study aims to translate and validate this instrument into Turkish, thereby contributing to the growing body of literature on obstetric mistreatment and serving as a valuable tool in medical education. Through the validation of this questionnaire in the literature, we seek to enhance awareness, education, and ultimately, the prevention of mistreatment within healthcare settings. The Perception of Obstetric Violence in Students Questionnaire (PercOV-S Q), originally developed and validated in Spanish and English to assess healthcare providers’ perceptions of obstetric violence, is crucial in identifying educational gaps and guiding training programs to reduce mistreatment. Validating the PercOV-S Q in multiple languages and applying it to trainees from diverse cultural backgrounds will underscore its universal reliability and contribute to understanding the global prevalence of obstetric mistreatment.
The PercOV-S Q comprises 33 positively worded questions, with participants’ perception of obstetric mistreatment measured using a 5-level ascending Likert scale (1: no OV; 5: considerable amount of OV). Each statement is scored on a scale of 1 to 5, with higher scores indicating increased perception of mistreatment.
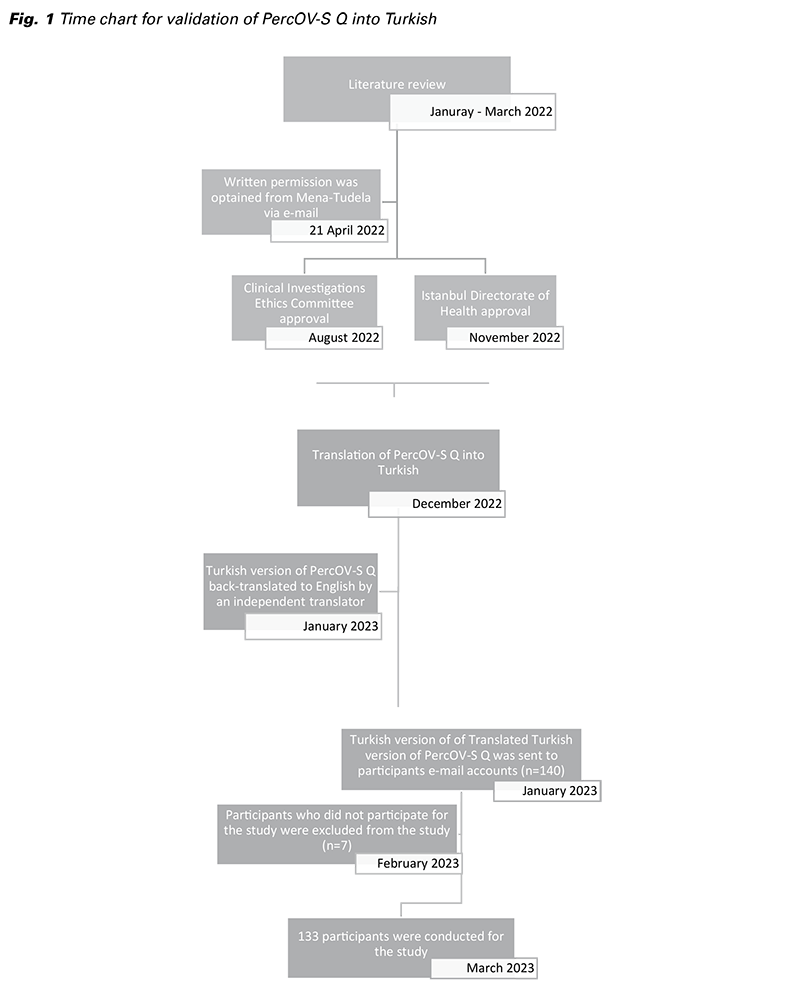
Following approval from the Clinical Investigations Ethics Committee on August 24, 2022 and the Istanbul Directorate of Health on October 13, 2022, the study commenced in November 2022 at our hospital. Ethical guidelines outlined in the Declaration of Helsinki were strictly adhered to throughout the research process. Written permission was obtained via email from Mena-Tudela for the utilization of the PercOV-S Q.
The communicative translation method was employed during the translation process to ensure precise contextual significance and linguistic accuracy, maintaining the original order of questions. The questionnaire was translated by a bilingual expert team fluent in both Turkish and English. It was then back-translated to English by an independent translator to ensure accuracy.
The study cohort comprised 140 obstetrics and gynecology residents, of whom 133 consented to participate in the study. Of these participants, 27.8% (n = 37) were female, and 72.2% (n = 96) were male. Among the female participants, 5.4% (n = 2) had given birth before. All residents in our study cohort were naïve Turkish speakers, possessed experience in obstetrics and gynecology clinics, had witnessed a birth, and had worked in the delivery room, having performed vaginal births under the supervision of obstetrics and gynecology specialists.
A web-based survey was developed to administer the PercOV-S Q. Participants were contacted via hospital email accounts and received a concise study overview along with a link to access the survey. Upon clicking the link, participants were directed to a platform where they were presented with an informed consent form followed by the questionnaire. Throughout the distribution of survey links and data collection, maintaining blinding to participant identities to minimize bias. For individuals who did or did not confirm to participate, their names were kept hidden at each stage of the study to prevent potential bias and preserve their autonomy. Time chart of the study is shown in Figure 1.
In line with the approach adopted by Mena-Tudela et al., participants in our study cohort, similar to medical, midwifery, and nursing students in their study, had attended an educational seminar on OV during their academic year (6). Therefore, our cohort comprised obstetrics and gynecology residents who had previously received education on OV, as part of the mother-friendly hospital program at our institution.
Principal component factor analysis with varimax rotation was employed for factor analysis. Items exhibiting a loading of 0.40 or higher on the principal components analysis were retained. Internal consistency was assessed using Cronbach’s alpha statistic, with a value of 0.70 indicating satisfactory internal consistency.
To determine the necessary sample size for factor analysis, a subject-item ratio between 4 and 10 is typically considered sufficient for ensuring stability. In our study, with 33 items within the PercOV-S Q, typically, a sample size of 10 participants per item is recommended for factor analysis, which would require 330 participants for a 33-item questionnaire. However, due to constraints, our sample size was 133, which still provided sufficient power for our analysis.
Out of the 140 eligible participants, 133 confirmed their participation and were included in the study. All participants were obstetrics and gynecology residents at our clinic, holding their primary medical degree from Turkey and speaking Turkish as their native language. As residents, they had all witnessed a birth, worked in the delivery room for at least one month, and performed vaginal births under the supervision of obstetrics and gynecology specialists. No issues with comprehension were identified regarding the questionnaire items. The viability of the factor analysis was confirmed through the Kaiser- Meyer-Olkin (KMO) test (p = 0.814) and Bartlett’s test for sphericity (X2 = 1898.897; p ≤ 0.001) (Tab. 1). We assumed no correlations between factors and thus adopted varimax rotation. The overall reliability of the questionnaire, as indicated by Cronbach’s Alpha score, was 0.840, supporting the internal consistency of the questionnaire and suggesting suitability for individual-level analysis in the Turkish language (Tab. 2), indicate that the Turkish version of the PercOV-S Q is a reliable and valid tool for assessing perceptions of obstetric violence among healthcare providers. The distribution of the participants’ responses to the items of the survey is demonstrated in Figure 2.
The variation in defining obstetric mistreatment during facility-based childbirth varies across different countries and institutions. This variability has led to significant oversight of this critical issue. As a result, accurately determining its prevalence and perception within healthcare settings, including those in Turkey, has become challenging. Addressing obstetric mistreatment requires a universal, inclusive definition to guide prevention efforts, particularly through education. This study contributes to this endeavor by demonstrating that the PercOV-S Q is a comprehensive and universal tool, validated for use in Turkish healthcare settings.
Obstetric mistreatment has been recognized as a violation of human rights, with legislation enacted in numerous countries since Venezuela‘s pioneering action in 2007 (2). Although the World Health Organization (WHO) did not explicitly use the term „obstetric violence“ in its 2014 statement, it provided clear examples of disrespect and abuse during facility-based childbirth. WHO emphasized the need for global measures to prevent and eradicate mistreatment during childbirth, generate data on respectful care practices, and prioritize training and education to combat obstetric violence (1). Recently, Chervenak et al aptly described ‚violence‘ as the deliberate use of physical force to cause harm, injury, or damage to another person, citing examples like physical assault, domestic violence, street fights, or acts of terror. In contrast, ‚mistreatment‘ is a broader term encompassing abuse, harm, or control exerted over another person, including nonconsensual medical procedures, verbal abuse, disrespect, discrimination, stigmatization, or neglect (7). We propose that the term ‚obstetric mistreatment‘ may be a more suitable descriptor for disrespectful and abusive mistreatment during facility-based childbirth.
While initial actions against obstetric mistreatment were predominantly observed in South American countries like Venezuela and Argentina, it is essential to recognize that this issue transcends regional boundaries. Recent literature from various countries, including the United States, Portugal, Spain, Ireland, South Africa, and India, underscores the global nature of obstetric mistreatment (8-13). For instance, a study by Reuther, M.L. investigated the prevalence of obstetric mistreatment in Germany and the Netherlands, revealing that 76.3% of participants experienced at least one component of a mistreatment during the childbirth (14). Furthermore, the American Psychiatric Association‘s updated Diagnostic and Statistical Manual of Mental Disorders (DSM-5) in 2013 acknowledges childbirth-related post-traumatic stress disorder (PTSD) as a subtype of PTSD, with risk factors such as instrumental delivery, episiotomy, severe pain during pregnancy, and inadequate labor care (15). Studies estimate the prevalence of childbirth-related PTSD following uncomplicated childbirth to range between 2.8% and 5.6% at 6 weeks postpartum (16,17).
In Turkey, awareness of obstetric mistreatment is increasing, yet the literature on this critical issue remains limited. Recent studies have revealed significant risk factors for obstetric violence and its association with postpartum depression. Additionally, in-depth analyses of women‘s personal experiences with mistreatment during childbirth have been conducted. Furthermore, studies have reported the prevalence of obstetric violence experienced by women, highlighting the pressing need for comprehensive strategies to address and mitigate this issue within healthcare settings (18-20). Our perspective offers a nuanced understanding of the interpretation of domains within the questionnaire. Contrary to the original delineation which assigns Domain 1 to actions perceived as mistreatment outside established protocols and Domain 2 to mistreatment within protocols, our viewpoint suggests a broader context. We assert that both Domain 1 and Domain 2 actions are inherent to the healthcare setting, particularly in labor rooms, often stemming from learned behaviors rather than intentional malice. We emphasize the pivotal role of education in shaping healthcare practices, particularly in obstetric care, as healthcare professionals operate within institutional norms and traditions. Our emphasis on education aligns with the understanding that behaviors are internalized from training and professional environments. By prioritizing comprehensive education and training initiatives, we can address the underlying causes of obstetric mistreatment, fostering a culture of evidence-based and respectful care. Our aim is not to assign blame but to underscore the significance of education in mitigating obstetric mistreatment. Through targeted education programs, healthcare providers can unlearn harmful practices and embrace patient-centered care, thereby enhancing childbirth experiences for women.
Future research should translate into different languages and validate the PercOV-S Q in various healthcare settings to assess its broader applicability. Additionally, integrating the validated questionnaire into educational curricula can help raise awareness and address obstetric mistreatment in clinical practice. Further studies should also investigate the impact of educational interventions on reducing abusive behaviors among healthcare providers.
One limitation of this study is the relatively small sample size and the specific cohort of nursing, midwifery, and medical students, which may affect the generalizability of the findings. Future studies should include larger and more diverse samples to validate the findings further.
Upon comparing the criteria of the MBFBF initiative with the items in the PercOV-S Q, it becomes evident that each statement in the questionnaire aligns with the MBFBF criteria. PercOV-S Q, created and validated by Mena-Tudela et al., serves as a unique tool. It assesses perceptions of mistreatment among students and healthcare professionals. Moreover, the Turkish version of the PercOV-S Q can serve as an educational resource. It raises awareness about inappropriate behaviors and inexpedient routine practices during the MBFBF adaptation process. Recognizing the paramount importance of education in nurturing a culture of respectful maternity care, we emphasize the WHO‘s plea and urge all stakeholders to actively participate in endeavors aimed at eliminating obstetric mistreatment (1). By placing education at the forefront and fostering collaboration, we can pave the way towards safer, more compassionate childbirth experiences for women worldwide.
This study successfully validated the Turkish version of the PercOV-S Q, confirming its reliability and internal consistency. These findings have significant implications for clinical practice, education, and policy, as the tool can enhance awareness and address obstetric mistreatment among healthcare providers. Also, our study suggests that, the PercOV-S Q can be adapted and validated in other languages, contributing to the global effort to combat obstetric mistreatment. Expanding the tool‘s use internationally can help standardize the assessment of perception and promote respectful maternal care worldwide.
This study received no financial or spiritual support from pharmaceutical companies or entities involved in the production of medical instruments or materials. There was no external funding that could potentially influence the evaluation process.
The authors declare no conflicts of interest with any individuals or entities involved in the research process, including pharmaceutical companies, scientific and medical committee members, or any other relevant parties.