











 Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.
Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.

Inguinal endometriosis is a form of extrapelvic endometriosis characterized by groin mass and periodic pain associated with the menstrual cycle. It is often accompanied with pelvic endometriosis, therefore symptoms include dysmenorrhea and lower abdominal pain. Since the rare occurrence it can be easily misdiagnosed prior to surgery. We present a case of a 27 years old patient with right sided painful groin mass which was firstly considered as an infectious necrotic lymphatic node. After pelvic examination and detection of a left ovarian endometrioma and further imaging examination of the groin region a suspicion of inguinal endometriosis was stated. Complete resection of the affected round ligament of the uterus with laparoscopic extirpation of endometrioma and peritoneal lesions was conducted with prompt recovery of the patient.
Endometriosis is a disease characterized by the presence of endometrial glands and stroma outside the uterus, primarily affecting the peritoneum and organs of the small pelvis (1). The precise prevalence of endometriosis in female adult population is not known, statistics suggest that 10-15% of women population in the world is affected (2). Inguinal endometriosis is defined as a rare extraperitoneal partial round ligament involvement with an incidence of 0.3 – 0.6% of patients affected by endometriosis (3). It was first described by Cullen in 1986 (4) with 133 reported cases in publications up till now (5). It typically presents as a small sized, tender and fixed inguinal mass with periodical exacerbation of pain during menstrual period. It is mostly located in the right groin and associated with pelvic endometriosis (6). The treatment consists of complete surgical excision of the lesion with the portion of the affected round ligament (7).
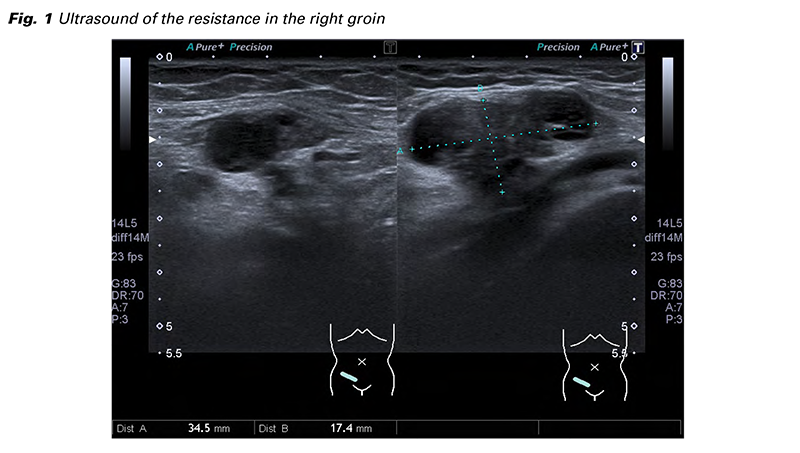
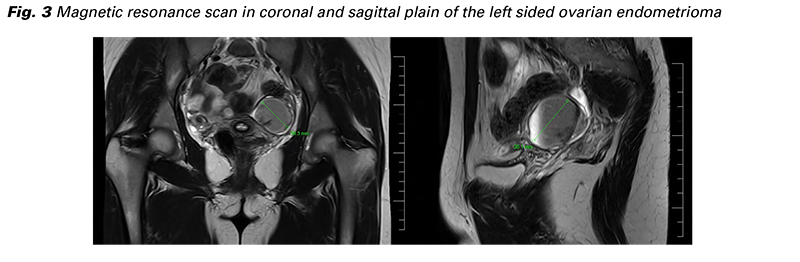
A 27 years old patient with known ovarian cysts seeks help at the Emergency department with a right sided lower abdominal pain. At the time she is in her ninth day of menstrual cycle, the location and characteristic of pain is similar as in her few last menstrual periods. She is nulliparous without any prior abdominal surgery or hormonal treatment, she has no significant medical history. During examination a hard resistance approximately 3x2 cm is palpated in her right groin of which she is aware of for a year and half, painful only during her menstrual period, but now continuously during the last month, mostly after long walks. On the ultrasound the mass showed as a mixed echogenic structure 34x17 mm with an anechogenic center of 13x11 mm resembling an infectious necrotic lymphatic node (Fig. 1). On vaginal ultrasound a 36x29 mm endometrioma of the left ovary was diagnosed with no further pathology in the pelvis. Further examination of the right inguinal region and gynecologic observation of the left sided ovarian endometrioma was recommended.
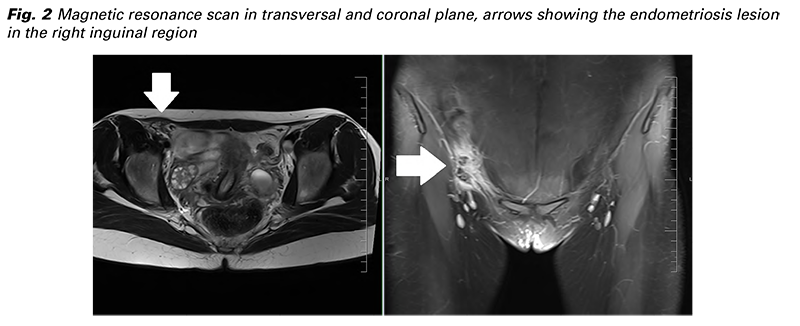
She was thoroughly examined at the Infectious disease department with wide laboratory testing (blood count with differential, HIV, syphilis, further common STDs, Lyme borreliosis, tularaemia, bartonellosis, toxoplasmosis), all negative. Based on the catamenial character of pain and the existence of the left sided endometrioma a differential diagnose of rare inguinal endometriosis was considered. A CT and MR scan was ordered finding the same solid, partly cystic, well bordered from the surrounding tissue structure, located ventrally of the femoral vessels at origin of the inferior epigastric artery in the inguinal canal (Fig. 2). The left sided ovarian endometrioma was described as well (Fig. 3). Laparoscopy with inguinal extirpation has been indicated.
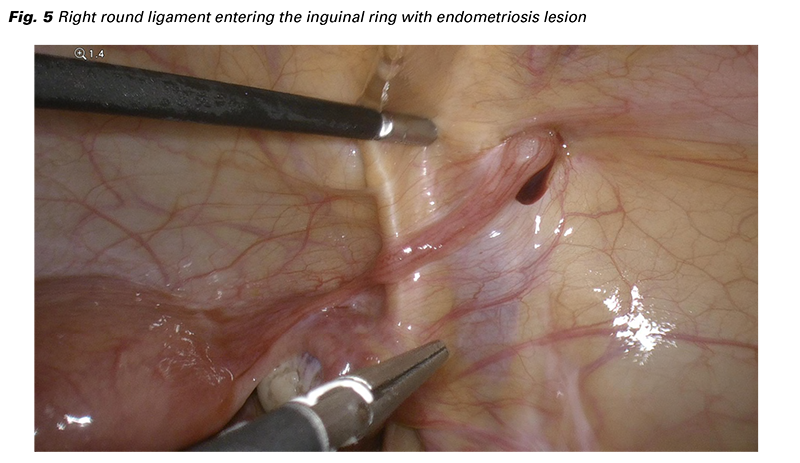
The intraoperative finding confirmed a left sided endometrioma (Fig. 4) and several small brown and blue peritoneal endometriosis lesions in the small pelvis (laterally from both uterosacral ligaments and in the posterior cul-de-sac) and also by the caecum. Visualizing the round ligament of the uterus, we have discovered a fibrotic nodule in the right distal part where entering the inguinal canal with slight dark blood leakage around (Fig. 5). The findings were described by the ENZIAN classification as P1, O2/0, T 0/0, A0, B0, C0, F (ligamentum teres uteri). The endometrioma of the left ovary has been completely extirpated followed by an adapting suture to restore the ovarian shape and eliminate bleeding and adhesion development. Excision of all the above
mentioned peritoneal lesions was achieved. The healthy end of the right round ligament just below the endometriosis lesion was marked with a single stitch to help to find the consecutive resection border from the inguinal canal. Irrigation and revision of any bleeding was done and the laparoscopy part has been finished.
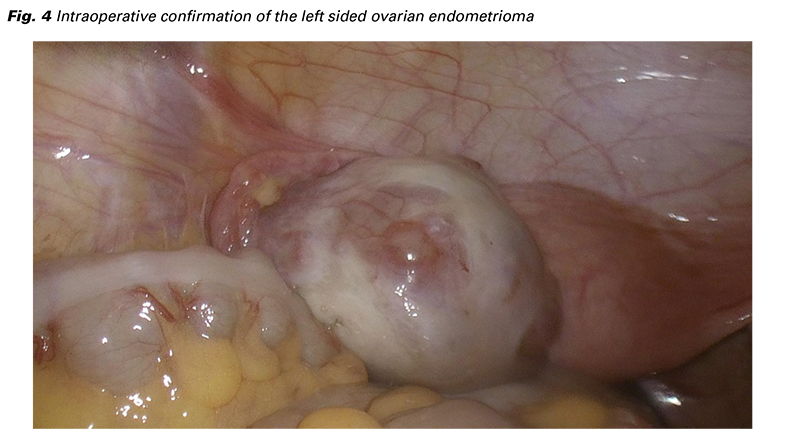
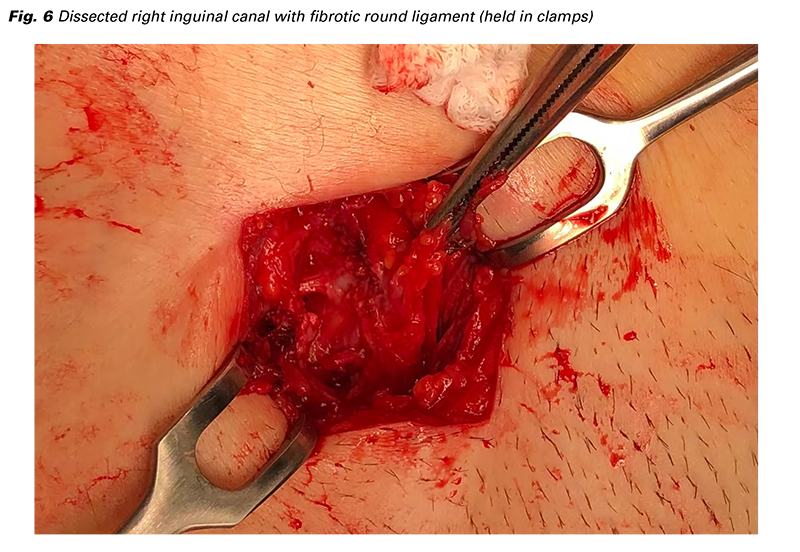
The general surgeon then explored the right groin area above the palpable resistance with the dissection of the inguinal canal to find a fibrotic round ligament extending all along to the previously put intraabdominal suture (Fig. 6). Full resection of the affected part of the round ligament was performed with fixation of the healthy end of the ligament to the peritoneum and closure of the groin. The surgery was without any complication, the patient recovered well and was discharged home the second postoperative day. Endometriosis was diagnosed in all the tissues sent to the pathology (endometrioma, peritoneal lesions, round ligament). No hormonal treatment was given because of her desire for pregnancy and is regularly followed in the outpatient clinic specializing in endometriosis treatment.
The above presented case includes all the common features for inguinal endometriosis the current literature offers. In the beginning, it is often misdiagnosed with other groin pathologies such as inguinal hernia, hemangioma, lymphadenopathy or hydrocele of canal of Nuck and confirmed later by histopathology (8,9). Taking consideration its rare occurrence, there is no consistent diagnostic algorithm to this date, which could directly lead to the proper diagnosis. The most distinct symptom that could indicate endometriosis is an unilateral inguinal mass with catamenial pain, however in the latest published review article this was noted only in half of the patients [10]. Ultrasound could show various images of the mass from predominantly solid to cystic or combined appearance (11). Furthermore MRI, PET-CT or even fine needle biopsy may be considered in more complex cases or when excluding metastatic lesions. Even this published case strongly suggested endometriosis based on its catamenial characteristics, other diagnosis were ruled out by interdisciplinary consultations and imaging methods. After discussion with the patient we have decided for surgical excision of the inguinal mass and extirpation of the ovarian endometrioma based on her painful symptoms. Alternative hormonal therapy could not be assigned regarding her desire for pregnancy. The right sided inguinal affection is interestingly more prevalent, unfortunately with no consistent or satisfactory explanation of this predominance in the literature (10). The pathophysiology of the inguinal endometriosis is at least as mysterious as endometriosis itself. The two most compelling theories are the embryological explanation, which refers to the remnants of early peritoneal cells (having the same embryological source as the endometrium cells) remaining in the inguinal canal and giving rise to endometrial cells by metaplasia (12), as well as the retrograde menstruation theory, when endometriosis migrates either through the inguinal ring and canal, or the patent canal of Nuck to the superficial inguinal soft tissues (13). The endometriotic lesion with blood around the pelvic part of the round ligament implies to the migration theory in our case. Finally it is worth to mention, that extraovarian endometriosis has a risk of malignant transformation as well (14), and even in an extremely rare occurrence of malignancy in inguinal endometriosis regarding it’s general infrequent incidence, there are individual cases published in the literature (15).
Inguinal endometriosis is a rarely seen condition but often associated with typical symptoms arising from its catamenial characteristic and location. As it is commonly concomitant with pelvic endometriosis, referral to the gynecologist for further assurance of the diagnosis is crucial. The treatment is surgical excision of the mass with laparoscopic pelvic exploration to address protentional endometriosis lesions. Our case report serves as an example of pitfall in uncertain diagnosis of groin mass in the beginning, but after proper examination surgery has been indicated with complete extirpation of endometriosis.
This publication has been supported by the Ministry of Defence, Czech Republic – MO1012.