











 Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.
Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.

Gartner’s duct cyst is an unusual vaginal cyst that develops from the Gartner’s duct, the residual embryonic structure of the caudal end of the mesonephric duct in females. Often discovered incidentally during routine pelvic exams on the anterior or lateral vaginal wall, these cysts typically exhibit no symptoms. Although the occurrence of Gartner’s duct cysts during pregnancy or at birth is exceedingly rare and has been scarcely documented in the literature, we encountered a pregnant patient who was referred to our hospital due to a protruding vaginal mass causing obstruction in the birth canal. Diagnosis was established through typical clinical examination and radiological findings, and after draining the Gartner’s duct cyst, a normal vaginal delivery was successfully performed.
The Gartner’s duct, a vestige of the Wolffian duct, develop cystic dilatation due to persistent glandular epithelial secretions, leading to the formation of Gartner’s duct cysts (GDC). Typically found along the anterolateral wall of the proximal third of the vagina (1). GDC may also coincide with abnormalities of the metanephric development. Notably, reports indicate that ectopic ureters, apart from establishing direct connections with the vagina and introitus, can communicate with GDC, resulting in urinary incontinence (2). In the classification of female congenital malformations of the genitourinary tract, the latest system by the European Society for Human Reproduction and Embryology / European Society for Gynaecological Endoscopy (ESHRE/ ESGE) categorizes Müllerian anomalies based on their anatomical status, with uterine, cervical, and vaginal anomalies being independently classified. An isolated GDC is classified as UO (Normal uterus) / CO (Normal Cervix) / V2 (Longitudinal non-obstructing vaginal septum) according to the ESHRE/ESGE system. Additionally, a GDC may be part of a complex distal mesonephric anomaly, such as unilateral renal agenesis and ipsilateral blind hemivagina syndrome, which would be classified as U3a (partial bicorporeal uterus) / C3 (unilateral cervical aplasia) / V2 (longitudinal obstructing vaginal septum) along with associated non-Müllerian anomalies (ectopic ureter) (3,4). While the majority of patients remain asymptomatic, those who do exhibit symptoms commonly experience dyspareunia, pelvic pain, a bulging pelvic mass, and urinary incontinence. The 2015 Thessaloniki consensus on the diagnosis of female genital anomalies, presented by ESHRE/ESGE, advocates the use of gynecological examination and 2D ultrasound as primary diagnostic tools for asymptomatic cases, widely acknowledged as suitable for most scenarios. In instances involving symptomatic complex anomalies, the consensus recommends 3D ultrasound imaging. Despite magnetic resonance imaging (MRI) offering superior diagnostic potential, its application is discouraged due to cost implications. However, it is proposed for investigating urinary anomalies during patient follow-up and for strategic planning in complex elective surgeries (5,6).
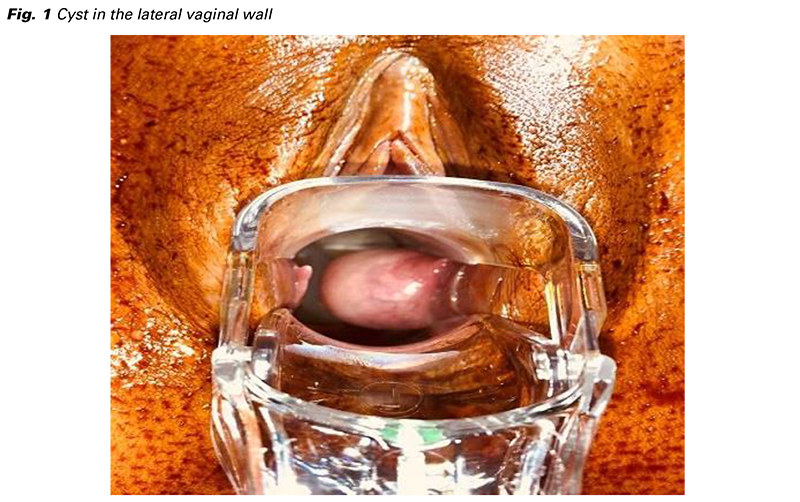
A 30-year-old woman, pregnant for the first time, was brought to our Emergency Department at 39 weeks of gestation with a primary diagnosis of a substantial vaginal mass obstructing the birth canal, rendering vaginal delivery impossible. Notably, she had no history of prior vaginal trauma, surgery, or any abnormal findings during past medical history or antenatal screening tests. Upon fetal ultrasound examination, a singleton live fetus was observed in cephalic presentation, with an estimated fetal weight of 3870 grams. During digital vaginal examination, a dilated cervix of 7 centimeters with 70% effacement and intact membranes was noted. A speculum examination revealed a solitary, tense cyst measuring approximately 5 centimeters in diameter along the lateral vaginal wall (Fig. 1). Transvaginal ultrasound displayed an anechoic cyst measuring 45 × 23 × 40 millimeters within the left vaginal wall, consistent with Gartner’s duct cyst (Fig. 2-3). Subsequent to admission to the labor and delivery ward, the patient underwent spontaneous labor with her informed consent. Once the cervix was fully dilated and effaced, the patient was positioned in lithotomy, and a 10 French drainage catheter was inserted into the cyst under local anesthesia. Following successful drainage of the cyst, a normal vaginal delivery was performed without any complications (Fig. 4). Informed consent was obtained from the patient for the publication of the case report.



During the intricate and evolving embryologic development of the female genital tract, the identification of a female genital malformation can be either an isolated Müllerian anomaly or part of a broader spectrum of anomalies (7). Therefore, an initial evaluation of Gartner’s duct cysts (GDC) should encompass a comprehensive patient history and physical examination. Imaging modalities such as MRI, computed tomography (CT), and ultrasonography (US) are valuable tools for further characterizing the lesion.
For definitive treatment of GDC, complete cyst excision is recommended, with the diagnosis confirmed through pathological examination. However, the current literature lacks a consensus regarding the most optimal surgical approach or conservative treatment and follow-up strategies. There exist successful case reports and series illustrating both surgical management and conservative treatment with follow-up (5,8).
In our specific case, with the primary objective of facilitating the birth of a woman with a vaginal mass, our approach was guided by physical examination findings, the cyst’s typical anatomical location, and ultrasound assessment. The strategy involved draining the cyst by inserting a simple catheter to enable a safe vaginal birth for both the mother and the newborn. The cytological examination of clear cyst fluid, revealing degenerated red blood cells, a few lymphocytes and polymorphonuclear leukocytes, with squamous cells, strongly supporting our initial diagnosis. A contrast-enhanced abdominal MRI performed six months postpartum indicated no uterine, cervical, or renal abnormalities. Furthermore, the GDC was not associated with any urinary tract abnormalities, such as an ectopic ureter. After thorough discussion with the patient and obtaining her consent, a long-term follow-up plan was selected.
To summarize, the differential diagnosis for a cystic lesion detected in the lateral wall of the vagina should include GDC. Our study highlights that conservative treatment can be a safe option for pregnant patients, emphasizing that GDC is not a contraindication for normal vaginal delivery, provided there is appropriate long-term follow-up.
This article has not been published elsewhere and that it has not been submitted simultaneously for publication elsewhere. The data that support the findings of this study are openly available in Aktuální Gynekologie a Porodnictví. No conflicts of interest between the authors and / or family members of the scientific and medical committee members or members of the potential conflicts of interest, counseling, expertise, working conditions, shareholding and similar situations in any firm. All coauthors have seen and agreed with the contents of the manuscript and there is no financial interest to report. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.