









 Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.
Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.

Background: Induction of labor is one of the most common procedures performed in the world of Obstetrics. Traditionally, labor induction is performed using prostaglandin and oxytocin. However, usage of corticosteroids nowadays is gaining a lot of interest regarding its effects on cervical ripening and shortening the physiological process of labor.
Aim of work: to evaluate the efficacy of intravenous dexamethasone versus vaginal misoprostol in enhancing cervical ripening and labor induction.
Patients and Methods: A randomized controlled clinical trial was carried out at Ain Shams University Maternity Hospital on (60) full term nulliparous pregnant women between 39 – 42 weeks undergoing induction of labor, during a period from April 01, 2019 to November 30, 2019. Pregnant women were divided into two groups; vaginal misoprostol (control) group and intravenous dexamethasone (experimental) group (30 cases each).
Results: Our study showed that the mean time interval (hours) from initiation of labor induction to initiation of active phase was statistically significantly shorter among the dexamethasone (experimental) group 7.36 ± 2.23 versus 12.20 ± 4.92 hours among the vaginal misoprostol (control) group (p-value < 0.001). Also, the mean time interval of the total duration between the induction of labor to successful vaginal delivery was statistically significantly shorter among the dexamethasone group 10.90 ± 4.17 versus 19.20 ± 5.62 hours among the vaginal misoprostol group (p-value < 0.001). The results of this study showed the rate of initiation of active phase and rate of successful vaginal delivery were higher in the experimental dexamethasone group than the control vaginal misoprostol control group but not significantly different.
Conclusion: Intravenous injection of 8 mg of dexamethasone before induction of labor is found to shorten the duration of labor induction by reducing the time interval between the initiation of labor induction and onset of active phase and the total duration from initiation of labor induction to delivery with no marked maternal or fetal complications.
Recommendations: Intravenous Dexamethasone can help cervical ripening and accelerate induction of labor. Further research should be taken in consideration with more population for more global evaluation.
Induction of labor is considered to be one of the problems of midwifery in which it is necessary to terminate pregnancy. The goal in the process of induction of labor is to achieve vaginal delivery by artificially stimulating uterine contractions before the spontaneous onset of labor. In order to decrease the time interval between induction process to delivery, the process of induction is usually initiated with cervical ripening (1).
Recently, it has been recognized that cervical and uterine changes involve the effect of prostaglandins, inflammatory mediators and other agents to take place. Understanding such agents and different biological processes have motivated scientists to explore different ways to provoke the process of labor. Induction of labor is considered to be one of the most common obstetrics technique and the fast growing medical method in the United States of America (2). Prostaglandins have been involved for a long time in the spontaneous onset of labor. The normal process of labor appears to result in inflammation which increase prostaglandins release. Prostaglandins produced in the myometrial tissue, contribute to the effectiveness of the uterine contractions during the process of labor and also may soften the cervix independent of uterine activity (3).
WHO recommends misoprostol and other prostaglandins for the process of induction of labor. If prostaglandins are not available, oxytocin alone or in combination with balloon catheter can be used, also balloon catheter alone may be used. Amniotomy alone is not indicated for induction by the WHO (4). On the other hand, the RCOG does not recommend misoprostol for labor induction outside the context of clinical trials, but it recommends Dinoprostone as the prostaglandin of choice as it have demonstrated a considerable efficacy and safety. In 2002, the FDA has approved the usage of misoprostol for induction of labor. ACOG and FIGO recommended the use of misoprostol with a dose of 25 mcg every 3-6 hours, for maximum 5 doses according to the majority of studies FIGO referred to. The ACOG states in its practice that amniotomy alone for labor induction may be unpredictable regarding its efficacy and may take a long time before the onset of spontaneous contractions. The RCOG as well as the WHO does not recommend amniotomy for labor induction, but recommend it for the management of labor delay. Other methods for labor induction include the use of corticosteroids and nitric oxide donors. Also mechanical methods such as cervical dilators and cheap nipple stimulation (5,6).
Interestingly, concentration of CRH levels has been shown recently to increase within the developing fetus during the last 12 weeks of gestation. Consequently these hormonal events and changes cause modified uterine contractility, trigger the membranes to produce more prostaglandins (PGE2 and PGF2α) and increase the estrogen content. Alteration of estrogen to progesterone ratio will eventually lead to increased contractile proteins expression. As a matter of fact, raised CRH near the end of gestation, confirms the existence of a placental-fetal clock (4,7).
Usage of corticosteroids is considered by various researchers and investigators to be one of the promising management protocols that recently have a rowing research interest to be considered as a future agent that could be implemented to accelerate the physiological process of labor. Although the underlying cellular and molecular processes are not fully understood, researchers performed studies on experimental animals that revealed the crucial role of cortisol secretion by adrenal glands in sheep fetuses and in fetuses of other experimental animals investigated in triggering the start of labor (8,9). Furthermore it has been observed by various research groups of investigators in a considerable fashion that glucocorticoids infusion into sheep fetuses triggers labor induction in a premature manner (9,10).
This study is a randomized controlled clinical trial that was conducted on 60 nulliparous pregnant women at 39 - 42 weeks gestation in the labor ward of Ain Shams University Maternity Hospital between April and November 2019, for the termination of their pregnancy. The inclusion criteria were nulliparous pregnant women 39 – 42 weeks of gestation, between 18 – 35 years, with Bishop score < 6, singleton fetus, cephalic presentation, with normal amniotic fluid, reassuring CTG and absence of malformations diagnosed by 2nd trimester ultrasound. Participants with diabetes, preeclampsia, fetal macrosomia, multiple pregnancy, breech presentation, rupture of membranes (ROM) and history of surgery on uterus were omitted. Women were recruited from the prelabor ward of our hospital after they had received information on the purpose and course of the study from the medical investigator and had provided the written consent then they were subjected to detailed history taking to rule out exclusion criteria, calculation of gestational age, general, abdominal and vaginal examination.
60 cases were divided into two groups using simple random distribution technique, Control group (A) “Vaginal misoprostol”: 30 cases undergoing induction of labor, received 25 mcg (1 tab) of vaginal misoprostol every 4 hours with assessment of Bishop score before each dose with total 4 doses. Women with soft cervix and those who progressed after misoprostol administration (Bishop score > 6), received an intravenous infusion of oxytocin. If no cervical ripening was achieved (Bishop score < 6) after the previous four doses, the outcome was considered to be failed labor induction and the infant was delivered by cesarean section. The experimental group (B) “Intravenous dexamethasone”: 30 cases undergoing induction of labor received a single dose of 8 mg (2 ml) of the product Dexamethasone sodium phosphate intravenously four hours before the initiation of augmentation of labor by intravenous infusion of oxytocin. Women with latent phase > 24 hours, the outcome was considered to be failed labor induction and the infant was delivered by cesarean section. We estimated the different time intervals among both groups including time interval between start of labor induction and active phase onset, active phase onset and time of delivery, and the total duration from the start of labor induction to delivery time. Moreover, we calculated the rate of patients who successfully entered the active phase of labor and those who successfully delivered vaginally. Also maternal adverse effects like uterine hyperstimulation, fetal distress and meconium-stained liquor were taken in consideration. The related information was recorded in checklists A and B. Using the statistical software SPSS - 23, this information was entered into a computer, the frequencies, means and standard deviations were calculated. The obtained results were analyzed by employing the student’s t–test and Chi-square test at P < 0.05.
Techniques and procedures used in conducting the study were thoroughly explained to the patients. Patients were given written informed consent forms and they participated in the study voluntarily.
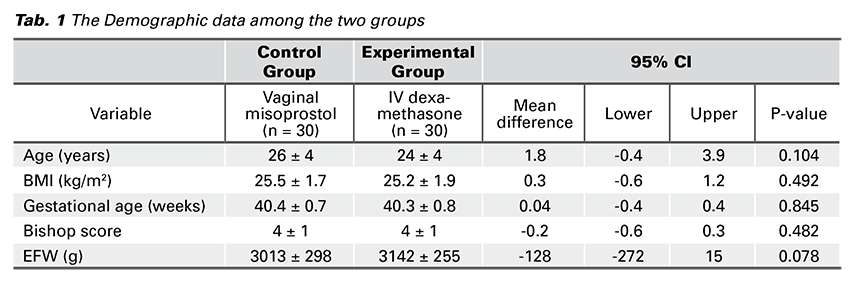
A total of 60 cases composed of 30 full term pregnant women in the control group and the same number in the experimental group participated in the study for induction of labor. Regarding the demographic data, there were no significant statistical differences between the two groups as regards the age (years), BMI (kg/m2), GA (weeks), Bishop score and EFW (grams) (p-value = 0.104, 0.492, 0.845, 0.482, 0.078, consecutively) (Tab. 1).
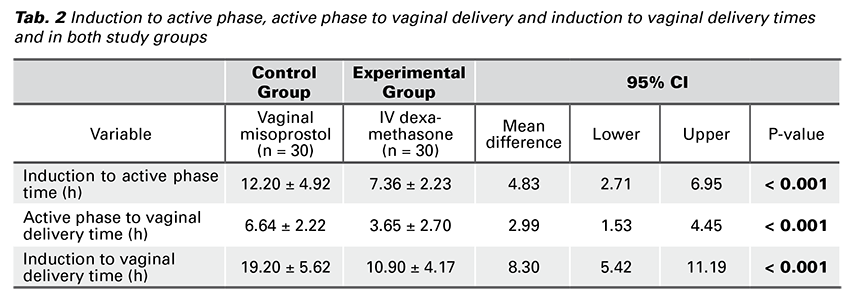
Interestingly, our study showed that the dexamethasone group has shorter time interval (hours) between initiation of induction of labor to active phase, active phase to vaginal delivery and from labor induction to vaginal delivery.
The mean time interval (hours) from initiation of labor induction to initiation of active phase was statistically significantly shorter among the dexamethasone group 7.36 ± 2.23 versus 12.20 ± 4.92 hours among the vaginal misoprostol group (p-value < 0.001). The mean time interval (hours) from initiation of active phase to vaginal delivery among the dexamethasone group was statistically significantly shorter 3.65 ± 2.70 hours than among the vaginal misoprostol group 6.64 ± 2.22 hours (p-value < 0.001).
Moreover, the mean time interval of the total duration between the induction of labor to successful vaginal delivery was statistically significantly shorter among the dexamethasone group 10.90 ± 4.17 versus 19.20 ± 5.62 hours among the vaginal misoprostol group (p-value < 0.001) (Tab. 2).
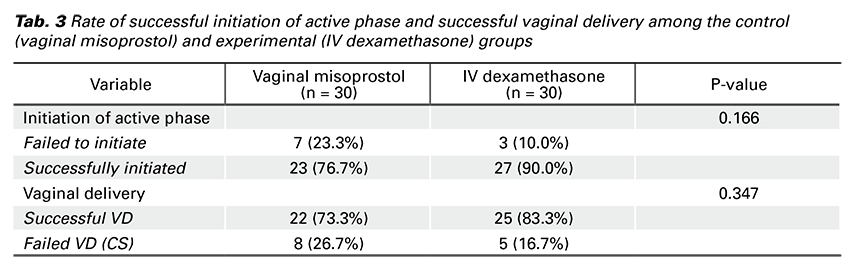
There were no significant statistical differences between the two groups as regard the rate of successful initiation of active phase and successful vaginal delivery (p-value = 0.166, 0.347, consecutively) (Tab. 3).
Furthermore, regarding maternal and fetal adverse outcomes; i.e. uterine hyperstimulation, fetal distress and meconium-stained liquor, were non-statistically significantly different between the two groups (p-value = 1.000).
In this study, intravenous dexamethasone (experimental) group showed shorter time interval (hours) between initiation of induction of labor to active phase onset, active phase to vaginal delivery and from labor induction to vaginal delivery, than that of the vaginal misoprostol (control) group.
In a study conducted by Laloha et al., who carried out a randomized double blind clinical trial on 172 primiparous participants visiting the maternity ward of the Kossar Hospital of the Qazvin University of Medical Sciences for the termination of their pregnancy who had Bishop scores of 4, and were in their 40th week of pregnancy then divided into dexamethasone (case) group and control group. The case group received a single dose of 8 mg dexa- methasone intravenously and the control group receive 2 ml of normal saline intravenously. Four hours later, induction of labor was started and performed by standard protocol using oxytocin so that the patient could enter active phase of labor (at least three uterine contractions in 10 minutes with cervical dilatation of 4 cm). They found that time interval between initiation of labor induction and onset of active phase of labor was statistically significantly shorter among the dexamethasone group 2.87 ± 0.93 versus 3.80 ± 1.72 hours among the control group. They concluded that intravenous dexamethasone reduces the time interval from induction of labor to onset of active phase of labor (11).
Our findings also regarding the vaginal misoprostol group, agreed with Silva et al., who carried out a retrospective cohort study of 412 pregnant women with > 40 weeks of gestation who were referred to a tertiary hospital in the southeast of Brazil with indication for labor induction. Labor induction was performed using 25 mcg tablets of vaginal misoprostol with Bishop scores < 6. The drug was inserted in the posterior fornix at a dosage of 1 tablet every 6 hours with a maximum period of 48 hours (8 tablets). In the cases in which labor was initiated, oxytocin was administered by a continuous infusion pump and those with absence of labor, induction was deemed unsuccessful after eight tablets with no cervical changes. They concluded that labor induction with vaginal misoprostol reduces the time interval between initiation of induction and onset of active and also reduces the total time interval from labor induction to delivery. However, unlike our study, they found that maternal age, basal Bishop score, the amount of misoprostol administered, and prior vaginal births were all associated with the successful induction of labor (p-value < 0.001) (12).
Our results also were consistent with Hajivandi et al., who carried out a single blind randomized clinical trial that was conducted on 100 nulliparous women who were referred to Amir Al Momenin Hospital in Ahvas. Study population comprised nulliparous pregnant women in their 40 – 42 weeks who were referred for termination of pregnancy. This study coincides with our inclusion criteria also including cases with basal Bishop score < 4. Cases were randomly divided into two groups. Study group received single dose of intramuscular dexamethasone (8 mg) 12 hours before classical induction by oxytocin was initiated. Control group was given 2 ml intramuscular injections of normal saline. They found that mean interval between labor induction and onset of active phase was statistically significantly shorter among the study group 3.1 ± 0.68 versus 4.2 ± 1.3 hours among the control group (p-value = 0.001). They concluded that intramuscular dexamethasone reduces the time duration from labor induction to onset of active phase of labor (13).
Kashanian et al. agreed with our results, carried out a double blind randomized controlled clinical trial upon 122 nulliparous pregnant women in 41 weeks of gestation and Bishop scores greater than or equal to 7 and were randomly assigned to receive a single dose of 8 mg of dexamethasone or placebo intramuscular 6 hours before initiation of labor induction. They found that more women in dexamethasone group entered active phase than women in the control group. Also interval between labor induction and onset of active phase in the dexamethasone group was shorter than that in control group (3.9 ± 1.5 versus 4.21 ± 1.8 hours, p-value = 0.001) (14).
Another team of investigators carried out a randomized research study to evaluate the effect of corticosteroids administration on childbirth. However they performed a different methodology in their research. The experimental group (n = 50) received 20 mg of dexamethasone diluted in a saline solution and used a Foley catheter infusion into the extra-amniotic space and only the extra-amniotic normal saline solution for the members of the control group (n = 48). The results showed that the mean time interval between induction of labor and the onset of active phase among the experimental group was statistically significantly shorter than among the control group (7.8 ± 3.1 versus 11.9 ± 3.9 hours). Also the time interval between induction of labor and delivery was shorter among the experimental group than the control group (11.9 ± 3.6 versus 14.5 ± 4.8 hours). Results of this study are similar to those of our study although the methodology of research used, is different (15).
However, reviews have yielded conflicting results regarding this issue. Kavanagh et al., reviewed a clinical trial conducted on 66 pregnant women in which the effects of prescribing intramuscular dexamethasone together with oxytocin was compared with the effects of using oxytocin alone. They raised the point that corticosteroids had no effect on inducing labor. Unlike our findings, the results that were reported by Kavanagh et al. found that corticosteroids had no role in softening the cervix or accelerating the physiological process of labor and that this method had not become popular and required further research and this may be attributed to usage of different route of administration of dexamethasone. Our results found that, contrary to their study, dexamethasone is effective in labor induction and causes ripening of the cervix (9).
Taking in consideration all studies that have been conducted (including our study), it appears that prescription of dexamethasone can play a role in enhancing cervical ripening and accelerating labor induction. Although we found that rate of successful initiation of active phase and that of successful vaginal deliveries among the dexamethasone group was more than that in the vaginal misoprostol group i.e. rate of successful initiation of active phase was 27 cases (90.0%) among dexamethasone group versus 23 cases (76.7%) among vaginal misoprostol group (n = 30, p-value = 0.166) and that of successful vaginal delivery among dexamethasone group was 25 cases (83.3%) versus 22 cases (73.3%) among the vaginal misoprostol group (n = 30, p-value = 0.347), there were no significant statistical differences between the two studied groups. It’s recommended that this study be repeated with larger sample size of population and that the maternal and fetal adverse outcomes be more investigated.
Intravenous injection of 8 mg of dexamethasone before induction of labor is found to shorten the duration of labor induction by reducing the time interval between the initiation of labor induction and onset of active phase and the total duration from initiation of labor induction to delivery with no marked maternal or fetal complications.
The main limitation of our study is the small sample size. Also, main perinatal/neonatal outcomes could have been collected to address the safety of the studied induction protocol. Also, other possible factors influencing labor time such as usage of peridural analgesia etc. could have been assessed.
Patient information and informed consent:
Consents of the patient was not required.
Subject confidentiality protection: Only the patients’ numbers and patients’ initials have been recorded in the Case Record Files. A personal patient identification list (Patient numbers with corresponding patients’ names) was maintained to enable records to be identified.
Protocol approval: Before the beginning of the study and in accordance with the local regulations followed, the protocol and all corresponding documents had been declared for Ethical and Research approval from The Ethical Committee of the Department of Obstetrics and Gynecology, Faculty of Medicine, Ain Shams University.
Study time: Recruitment of data began once the protocol was approved by the Research and Ethical Committee of the Department of Obstetrics and Gynecology.
Intravenous dexamethasone can help cervical ripening and accelerate induction of labor. Further research should be taken in consideration with more population for more global evaluation.